Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Trichoscopy — extra information
Trichoscopy
Author: Dr Ahmed Sadek, Cairo Hospital for Dermatology & Venereology (Al-Haud Al-Marsoud), Egypt. March 2022.
Contributors: Dr Dalia Hossam, Dr Radwa Magdy, Dr Nehal Saied, Dr Noha Hashem, Dr Safaa Yehia Negm, Dr Moshera Saied El Bahrawy, Dr Amira Ragab, Dr Amal Wagih, Dr Haidy El-Hussieny, Dr Mona Ragib, Dr Hala Amer. Copy edited by Gus Mitchell. March 2022
Introduction
Introduction
Value of trichoscopy
Perifollicular skin
Introduction
The dermatoscope is a non-invasive diagnostic device that allows better recognition of morphologic structures not visible to the naked eye. Current use of the dermatoscope has widened, and the vast majority of dermatologists and some general practitioners have embraced dermoscopy as the gold standard to differentiate melanoma from other pigmented skin lesions.
Dermoscopy has become valuable in the recognition of non-pigmented skin lesions, as well as inflammatory dermatoses, and trichoscopy is being adopted as a valuable technique in evaluating the hair not only on the scalp but on the brows and hairy areas elsewhere.
Other DermNet pages on trichoscopy include:
- Trichoscopy of scalp infestations
- Trichoscopy of inflammatory conditions
- Trichoscopy of localised cicatricial hair loss
- Trichoscopy of localised noncicatricial hair loss
- Trichoscopy of generalised noncicatricial hair loss
- Trichoscopy of genetic hair shaft disorders
What is trichoscopy?
Trichoscopy involves examination of the scalp and hair using a handheld or a videodermoscopy device. Examination with a dermatoscope (trichoscope) can reassure patients that they have received a thorough scalp examination and provide the clinician with invaluable in vivo information about scalp and hair shaft pathology.
Hand-held trichoscope

A conventional dermatoscope in use for trichoscopy
Videodermoscopy is a new and valuable tool in assessing hair and scalp disorders. Surface and subsurface microscopic views provide a previously unrecognized clinical perspective on disease, features seen with the naked eye are visibly enhanced, and patterns of disease that help in diagnosis are readily visualized.
The images are acquired by computerized polarized-light videomicroscopy using lenses with factors of magnification at 10× increments. Both epiluminescent and non-epiluminescent modes were employed. Alcohol gel is used as the interface solution. Captured images are digitalised and displayed on a high-resolution monitor in real-time. Selected images can be stored on a computer for serial assessment over time.
Videotrichoscope

Videotrichoscopy apparatus
What is the value of trichoscopy?
Trichoscopy represents a valuable, non-invasive and low-cost technique which can be of help in diagnosis of most hair and scalp diseases, allowing visualisation of the hair and scalp at x20 to x160 magnifications.
Images can be recorded digitally either using a separate digital camera connected to the trichoscope, or a built-in digital imaging system.
It can help to distinguish scarring versus non-scarring alopecia, early androgenetic alopecia versus telogen effluvium, and predict prognosis of alopecia areata.
Many studies describe its application in randomly selected patients suffering from hair loss, not only as a diagnostic tool but also in monitoring treatment response. Other uses include guiding selection of the optimum site of scalp biopsy and teledermoscopy for case discussion and second opinions.
Current research is focusing on trichoscopy of:
- Non-cicatricial alopecia
- Cicatricial alopecia
- Hair shaft disorders
- Inflammatory scalp diseases
- Infectious scalp diseases.
Special considerations
- Hair washing may eliminate important physical signs. Ask patients not to wash their hair for at least 2–3 days before trichoscopic examination.
- Patients with intense scaling may be asked to apply a keratolytic product to the scalp for 1–2 weeks, and then trichoscopy may be performed again. Removing the scaly coating layer improves visibility of the blood vessels.
- Objects on the scalp that may hinder diagnosis include dirty dots (in children), leftover hair dye, makeup foundation, textile fibres, or cosmetic hair fibres.
- Eyebrows and eyelashes are best inspected with a non-contact dermoscope. Never use alcoholic immersion fluids for eyebrows and eyelashes.
- Ultraviolet-enhanced trichoscopy (UVET) may facilitate the diagnosis of diseases that exhibit fluorescence on Wood light.
Trichoscopic structures & patterns
Trichoscopy allows four basic structures to be recognized:
- Follicular openings
- Perifollicular skin
- Hair shafts
- Vascular structures.
All structures must be examined thoroughly and any report should include the normal and the abnormal findings as the collective data interpretation leads to a more accurate diagnosis.
Follicular openings (dots)
Trichoscopy is a useful tool in assessment of the hair follicle condition whether:
- Normal
- Fibrotic
- Empty
- Plugged with keratin
- Containing hair residues
- Absent.
Follicular openings are classified according to the following criteria.
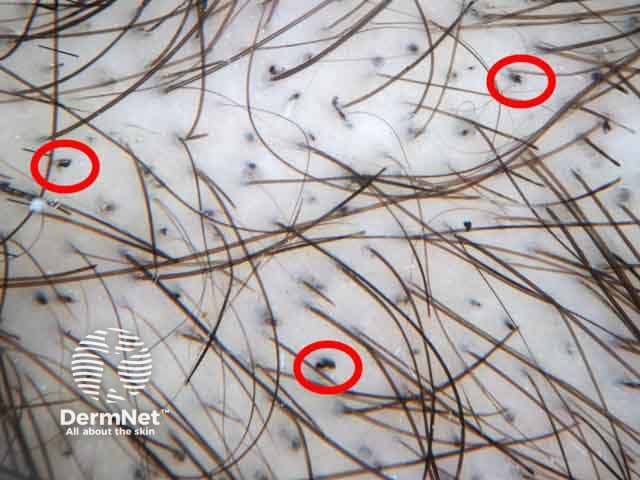
Size and distribution
- Small and uniform with symmetric distribution usually denote non-cicatricial alopecia.
- Large and irregular with asymmetric distribution usually denotes underlying cicatricial alopecia.
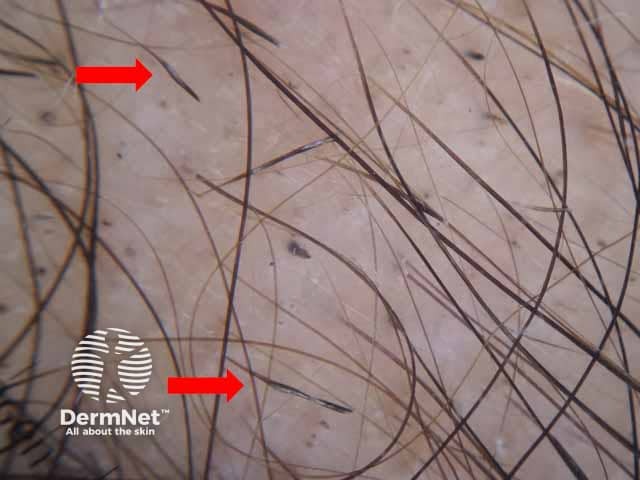
Follicular openings

Dermoscopic image of noncicatricial alopecia areata presenting with small, uniform, regularly distributed follicular yellow dots

Dermoscopic image of lichen planopilaris presenting with irregularly distributed follicular openings (red arrows) denoting scarring (cicatricial) alopecia
Colour
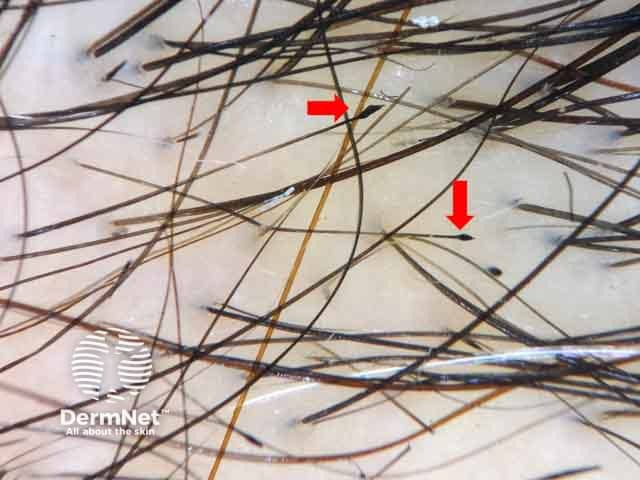
A black dot (previously called a cadaverized hair) is a term used to describe a follicular opening which contains remnants of pigmented hairs broken at the scalp level.
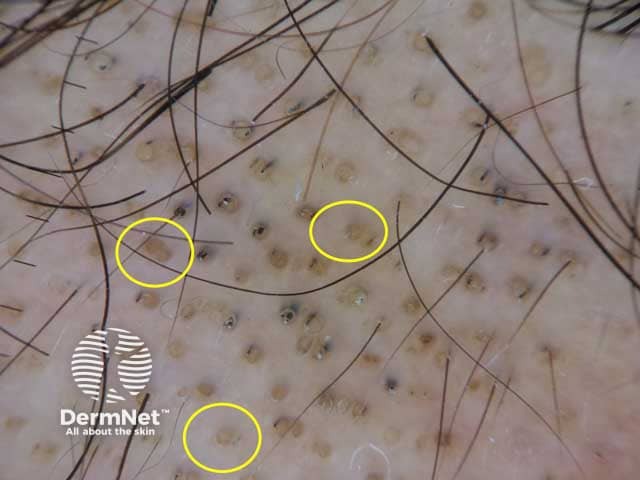
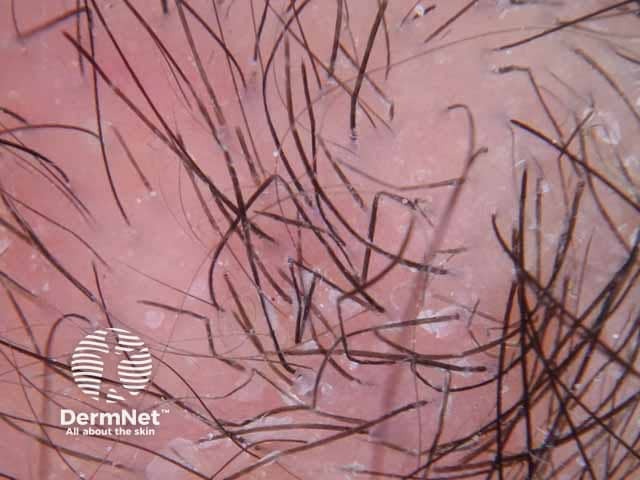
Black dots

Trichotillomania showing black dots; follicular openings with remnants of pigmented hairs broken at scalp level
Causes of black dots
- Inflammatory process eg, alopecia areata, dissecting cellulitis
- Hair shaft invasion eg, tinea capitis
- Mechanical injury eg, trichotillomania and traction alopecia
- Drug cytotoxicity eg, chemotherapy-induced alopecia.
Yellow dots represent follicular infundibulae filled with keratin with no hair shafts. They are detected in different cicatricial and non-cicatricial disorders.
Yellow dots
Dermoscopic image of alopecia areata showing yellow dots; follicular infundibulae are filled with keratinous material with no hair shafts. Black dots are also presented. (AA-patient2)
Causes of yellow dots
Causes of white dots
- Normal finding is sometimes seen in the scalp of individuals with Fitzpatrick skin types IV, V, and VI. The white dots are uniform in size and shape with dark pigmented reticular background, this pattern is described by the term ''honeycomb pattern''.
White dots

Dermoscopic image of a patient with dark skin phototype showing honeycomb pattern; white-coloured follicular opening with reticular background.
Fibrosis following the destruction of hair follicles, such as in lichen planopilaris, appears variable in size and shape and may become confluent forming structureless white areas. In severe alopecia areata, cumulus-like white dots representing confluent fibrosis of follicles are reported.
Red dots were described mainly in discoid lupus erythematosus. Many authors believe that the presence of red dots is a good prognostic factor denoting the possibility of hair regrowth.
Pink dots are occasionally seen in the eyebrow area in patients with frontal fibrosing alopecia.
Hair shafts
The normal human hair shaft cross-section is divided into three zones; the medulla, the cortex, and the cuticle, with different variations among races.
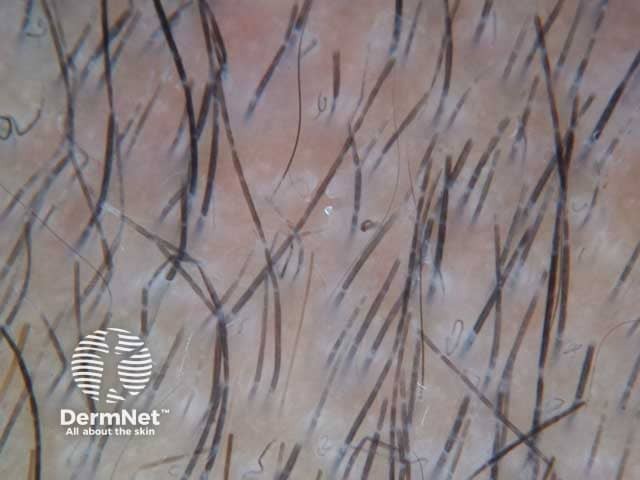
The normal hair shafts are uniform in thickness and colour. Using trichoscopy of normal hair shafts, authors describe two types of hair:
- Terminal hair is thick and medullated, representing 90% of scalp hair
- Vellus hair is hypopigmented and non-medullated, representing 10% of normal scalp hair.
Trichoscopy is used widely to detect different hair shaft, shape, and thickness disorders and diagnosis of their causative diseases. Abnormalities of shape can be classified according to the underlying cause:
Genetic
Fractured hairs
- Trichorrhexis invaginata is commonly seen in patients with Netherton syndrome.
Narrowings
- Monilethrix is defined as regularly distributed nodes and internodes along the hair shafts. These nodes represent the normal hair shaft thickness, while the internodes are the constriction points at which hair shafts tend to fracture.

Dermoscopic image of monilethrix; regularly distributed nodes and internodes along the hair shafts
Node-like appearance
- Trichorrhexis nodosa is described as nodular thickening in which the hair shaft splits longitudinally to many hair fibres.
Curls and twists
- Zigzag hairs occur due to focal weakening of the hair shaft which is observed in trichorrhexis nodosa.
- Pili torti shows flattened shafts and hairs twisted on their own axis.
- Woolly hairs represent thin hypopigmented tight curly hairs.
Bands
- Pili annulati is characterized by alternating bright and dark bands along the hair shaft due to the presence of air filled cavities.
Acquired
Fractured hairs
- Trichoptilosis is used to describe distal splitting and damage of the hair shaft. It may be seen in patients with alopecia areata and in individuals using cosmetic damaging agents such as straighteners.
- Irregular fractures caused by mechanical force.

Dermoscopic image of trichoptilosis; distal splitting and damage of the hair shaft and extravasated blood in a patient with lichen simplex chronicus.
Narrowings
- Monilethrix-like hairs (Pohl-Pinkus constriction) in which irregular fusiform narrowings occur following chemotherapy or caused by long-standing diseases such as alopecia areata.
- Pseudo-monilethrix is characterized by irregular flattening of hair shafts. The aetiology of pseudomonilethrix is controversial; some authors describe it as artifactual, due to excessive use of hair cosmetics.
- Tapered hair refers to a thin shaft at the proximal end with normal thickness at the distal one. It is a common finding in alopecia areata.
- Exclamation mark hairs are short and hypopigmented at the proximal end and thicker and darker at the distal end. Such hairs are one of the most characteristic features of alopecia areata. Sometimes exclamation mark hairs are observed in trichotillomania. In such cases, they appear dark at the proximal end and flat at the distal end.
Dermoscopic image of long standing alopecia areata showing Pohl-Pinkus constriction; irregular fusiform narrowings of the hair shaft
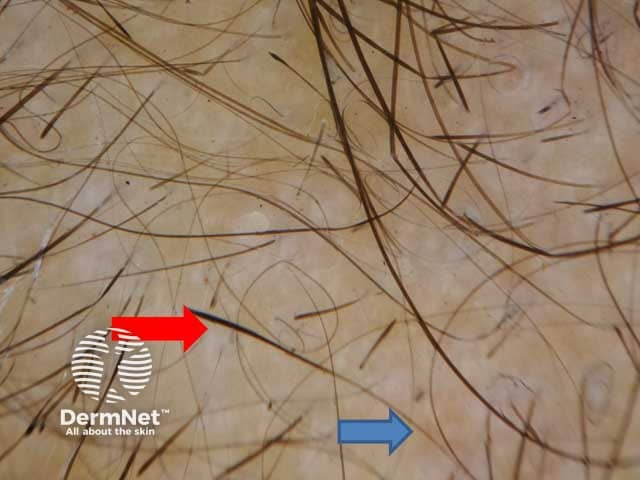
Thinning of the hair shaft at the proximal end (blue arrow) with normal thickness at the distal end (red arrow)

Dermoscopic image of alopecia areata presenting with exclamation mark hairs
Node-like appearance
- Trichonodosis is an acquired condition in which a single or double knot is observed along the hair shaft. It occurs commonly in individuals with short curly hair.
- Trichorrhexis nodosa is seen in patients with physical, chemical, or thermal trauma, scalp pruritus, seborrheic dermatitis, and biotin deficiency.
Curls and twists
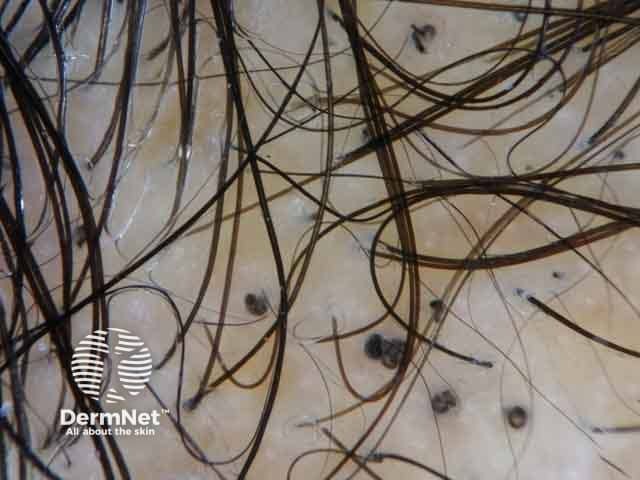
- Pigtail hairs are short twisted hairs representing regrowing hairs.
- Coiled hairs occur in trichotillomania and tractional alopecia due to the mechanical pulling forces exerted on the hair shafts.
- Comma hair is one of the pathognomonic features of tinea capitis
- Corkscrew hairs are the hallmark of tinea capitis.
- Zigzag hairs can be observed in tinea capitis and alopecia areata.
- Hook hairs are described in patients with trichotillomania.
- Pili torti hairs can be observed in alopecia areata, cicatricial alopecia, hair transplantation, and trauma.

Dermoscopic image of alopecia areata showing a pigtail hair: short twisted hair representing a regrowing hair

Dermoscopic image of tinea capitis presenting with comma hairs
Dermoscopic image of tinea capitis presenting with corkscrew hairs
Dermoscopic image of tinea capitis showing zigzag hairs; focal weakening of the hair shaft in a male child

Trichotillomania showing hook hair (red arrow)
Bands
- Morse code-like hair shows interrupted hairs with multiple bands along the hair shaft that occurs in patients with tinea capitis caused by Microsporum canis species.
Morse code hairs
Dermoscopic image of tinea capitis showing morse code–like hair; interrupted hairs with multiple bands along the hair shaft in a female child.
Short hairs
- They can be upright regrowing terminal hairs.
- Dark lines are present commonly in alopecia areata incognito.
- Tulip hair — often used to describe a hair shaft with a darker distal end which occurs mainly in trichotillomania and to a lesser extent in alopecia areata.
- Block hairs are very short hairs with a horizontal distal end, which may be observed in tinea capitis.
- Broom hairs represent multiple thin short hairs emerging from a single hair follicle. They can be observed in different types of cicatricial and non-cicatricial alopecias.
- Flame hairs are commonly observed in trichotillomania. They represent the hair remnants of recently pulled hairs.
- V-sign represents two hair shafts emerging from the same follicle and cut at the same level. This sign can be observed in trichotillomania.
Dermoscopic image of trichotillomania showing flame figures; hair remnants of recently pulled hairs
Dermoscopic image of trichotillomania showing tulip hair; hair shaft with darker distal end

Trichotillomania showing V-sign that represents two hair shafts emerging from the same follicle and cut at the same level
Abnormalities in hair shaft thickness occur in androgenic alopecia due to miniaturization.
Hair casts represent detached hyperkeratotic and parakeratotic cells of the inner root sheath which surrounds the hair shaft. Different conditions show peritubular casts including:
- Inflammatory disorders eg, psoriasis, seborrhoeic dermatitis, folliculitis decalvans, and lichen planopilaris
- Mechanical trauma eg, traction alopecia
- Autoimmune disorders eg, pemphigus vulgaris.
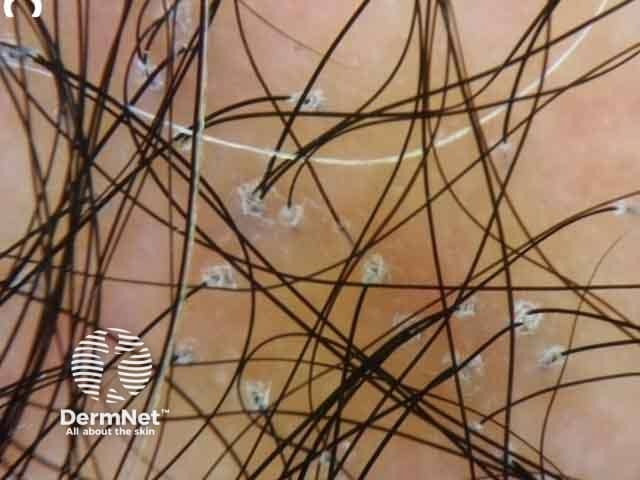
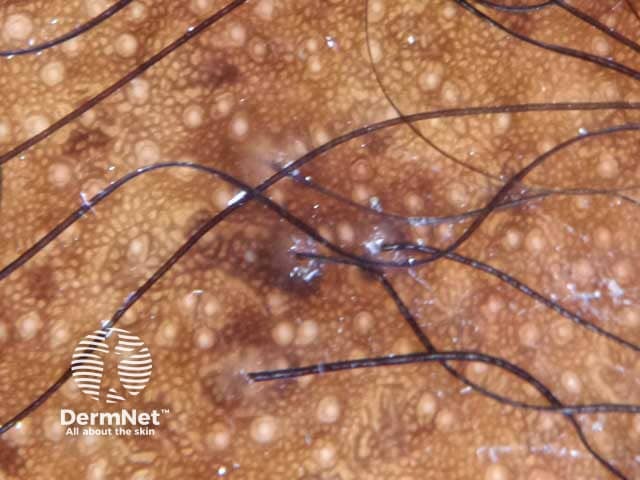
Hair cast
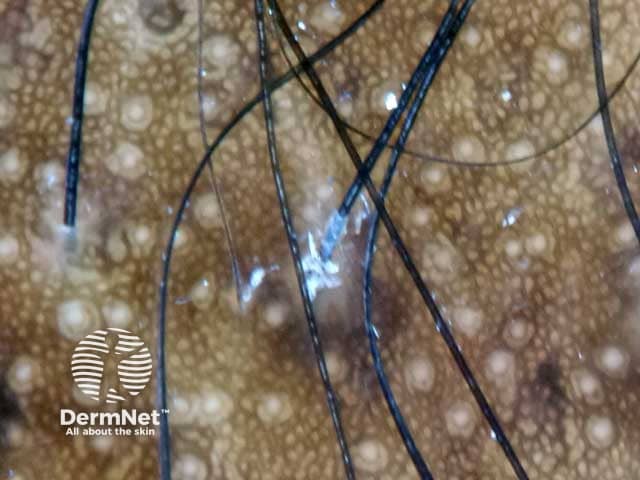
Dermoscopic image of hair cast represented by detached hyperkeratotic and parakeratotic cells of the inner root sheath
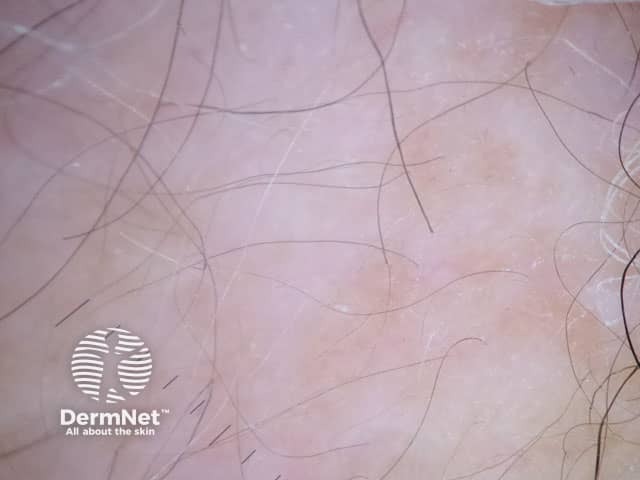
Perifollicular skin
Examination of perifollicular skin provides significant clues that help in the diagnosis of different scalp disorders. Assessment of scalp texture is helpful to differentiate cicatricial from non-cicatricial alopecias.
Trichoscopic features that may be observed in perifollicular skin include; scales, areas of different colours, discharge, vascular structures, and some others.
Texture
Scalp atrophy is a clinical finding that can be confirmed using trichoscopy. In patients with alopecia areata who have received prolonged use of steroid injections, prominent vessels, and visible hair bulbs with ivory-coloured areas (due to the steroid solution excipients) are observed.
Scales
Scales are classified according to their distribution into:
- Diffuse mild scaling may occur in healthy individuals with dry skin while moderate or severe scaling occurs in different inflammatory skin conditions. In psoriasis, scales are silver-white and dry, while in seborrheic dermatitis they appear yellowish, thick, and greasy.
- Localized perifollicular scaling is observed in frontal fibrosing cicatricial alopecia and represents a sign of activity in lichen planopilaris.
Dermoscopic image of a scaly scalp showing perifollicular scales in a female patient with lichen planopilaris
Colour
Perifollicular skin may show different colours, each suggesting an underlying specific condition.
- Brown colour; diffuse brown colour which is also called the honeycomb pattern is a normal finding in individuals with dark skin colour. Perifollicular pigmentation occurs in female and male androgenetic alopecia, and telogen effluvium. Scattered pigmentation occurs in discoid lupus erythematosus and lichen planopilaris.
- White areas often denote fibrosis, cicatricial alopecia, detached epidermis, or oedema.
- Pink areas are described in early fibrosis in cicatricial alopecia.
Dermosocpic image of a honey comb pattern in a female of African ethnicity
Dermoscopic image of the scalp on a female patient with longstanding alopecia areata showing white areas denoting fibrosis
Scarring alopecia with loss of follicular openings, sclerosis and telangiectatic vessels due to discoid lupus erythematosus
- Yellow areas are observed in dissecting cellulitis, follicular pustules, and bacterial infection.
- Red colour is a sign of inflammation or extravasation of blood.
- Salt and pepper areas are described in patients with systemic sclerosis.
- Salmon-coloured halos surrounding the follicular ostia are reported to be associated with systemic amyloidosis. They represent the amyloid deposits.
- Blue-white veil corresponding to hyperkeratosis overlying interface changes is reported in discoid lupus erythematosus.
- Orange colour is observed in patients with sarcoidosis representing granulomas located in the superficial dermis.
Discharge
Yellow and yellow-red discharge is observed in folliculitis decalvans, bacterial infections, dissecting cellulitis, or inflammatory tinea capitis.
Vascular structures and patterns
In order to examine vascular structures of the scalp, non-contact or videodermoscopy with higher magnification is preferred. Vascular structures detected using trichoscopy are widely variable in morphology and distribution according to the underlying causative disorder.
Inflammatory disorders
- Seborrhoeic dermatitis lesions may show thin arborizing vessels.
- Psoriasis lesions show dotted and glomerular vessels arranged in clusters or sometimes homogeneously distributed. Signet ring vessels were also observed by videodermoscopy in psoriatic patients.
- Discoid lupus erythematosus plaques show thick arborizing vessels.
- Systemic sclerosis shows a polymorphous pattern of blood vessels including arborizing vessels seen between avascular areas, spider vessels, and capillary loops in the frontal area.
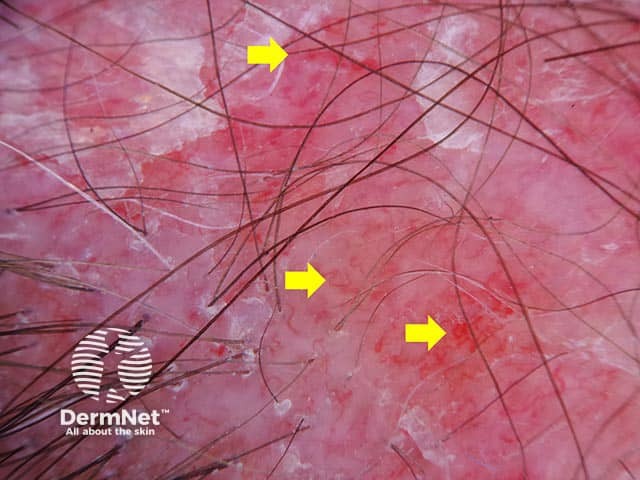
Dermoscopic image of discoid lupus erythematosus showing arborizing blood vessels (yellow arrows)
Autoimmune bullous diseases
- Dotted vessels with a white halo, linear serpentine vessels, or haemorrhagic areas may occur in pemphigus vulgaris.
Others
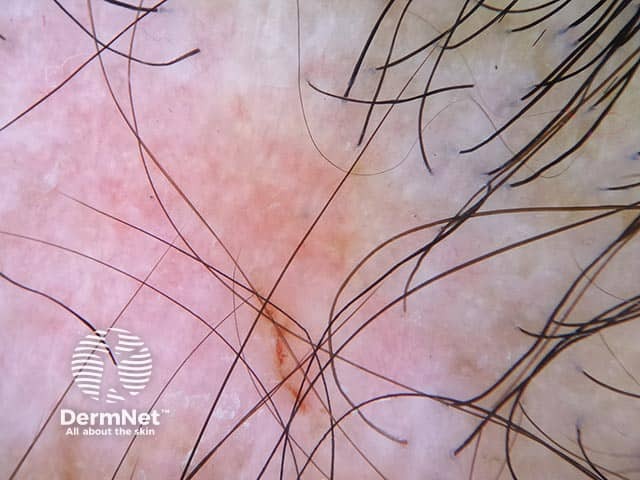
- Starburst pattern occurs in patients with folliculitis decalvans.
- Visible hair bulbs arranged radially in non-bullous aplasia cutis congenita.
- Perifollicular haemorrhage and hair powder in patients with trichotillomania.
Aplasia cutis congenita

Dermoscopic image of aplasia cutis congenita showing visible hair bulbs on the scalp of a female child.
Bibliography
- Bakos RM, Blumetti TP, Roldán-Marín R, Salerni G. Noninvasive Imaging Tools in the Diagnosis and Treatment of Skin Cancers. Am J Clin Dermatol. 2018;19(Suppl 1):3–14. doi:10.1007/s40257-018-0367-4. Journal
- Hu R, Xu F, Han Y, et al. Trichoscopic findings of androgenetic alopecia and their association with disease severity. J Dermatol. 2015;42(6):602–7. doi:10.1111/1346-8138.12857. Journal
- Kibar M, Aktan Ş, Bilgin M. Dermoscopic findings in scalp psoriasis and seborrheic dermatitis; two new signs; signet ring vessel and hidden hair. Indian J Dermatol. 2015;60(1):41–5. doi:10.4103/0019-5154.147786. Journal
- Kibar M, Aktan Ş, Lebe B, Bilgin M. Trichoscopic findings in alopecia areata and their relation to disease activity, severity and clinical subtype in Turkish patients. Australas J Dermatol. 2015;56(1):e1–e6. doi:10.1111/ajd.12102. Journal
- Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67(5):1040–8. doi:10.1016/j.jaad.2012.02.013. Journal
- Piccolo V. Update on Dermoscopy and Infectious Skin Diseases. Dermatol Pract Concept. 2019;10(1):e2020003. Published 2019 Dec 31. doi:10.5826/dpc.1001a03. PubMed Central
- Rakowska A, Slowinska M, Kowalska-Oledzka E, et al. Trichoscopy of cicatricial alopecia. J Drugs Dermatol. 2012;11(6):753–8. PubMed
- Rakowska A, Slowinska M, Kowalska-Oledzka E, Rudnicka L. Trichoscopy in genetic hair shaft abnormalities. J Dermatol Case Rep. 2008;2(2):14–20. doi:10.3315/jdcr.2008.1009. PubMed Central
- Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol. 2006;55(5):799–806. doi:10.1016/j.jaad.2006.04.058. Journal
- Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol. 2008;7(7):651–4. PubMed
- Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5(4):82–8. doi:10.3315/jdcr.2011.1083. PubMed
- Tosti A, Preface in Dermoscopy of Hair and Scalp Disorders with clinical and pathological correlations, Taylor & Francis Group, Florida, 2007, pp. vii.
- Trüeb RM, Dias MFRG. A Comment on Trichoscopy. Int J Trichology. 2018;10(4):147–9. doi:10.4103/ijt.ijt_13_18. Journal
On DermNet
- Dermoscopy
- Hair shaft defects
- Trichoscopy of scalp infestations
- Trichoscopy of inflammatory conditions
- Trichoscopy of localised cicatricial hair loss
- Trichoscopy of localised noncicatricial hair loss
- Trichoscopy of generalised noncicatricial hair loss
- Trichoscopy of genetic hair shaft disorders
