Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Trichoscopy of generalised noncicatricial hair loss — extra information
Follicular disorder Diagnosis and testing
Trichoscopy of generalised noncicatricial hair loss
May 2022
Author: Dr Ahmed Sadek, Dermatologist, Cairo Hospital for Dermatology & Venereology (Al-Haud Al-Marsoud), Egypt (2022)
Contributors: Dr Dalia Hossam, Dr Radwa Magdy, Dr Nehal Saied, Dr Noha Hashem, Dr Safaa Yehia Negm, Dr Moshera Saied El Bahrawy, Dr Amira Ragab, Dr Amal Wagih, Dr Haidy El-Hussieny, Dr Mona Ragib, Dr Hala Amer (2022)
Edited by the DermNet content department
Introduction
Androgenetic alopecia
Alopecia areata
Diffuse alopecia
Telogen effluvium
Anagen effluvium
Tractional alopecia
Introduction
Generalised noncicatricial hair loss is a non-scarring, potentially reversible type of hair loss.
Main causes of generalised noncicatricial alopecia:
- Androgenetic areata
- Alopecia areata
- Diffuse alopecia
- Telogen effluvium
- Anagen effluvium
- Tractional alopecia.
Androgenetic alopecia
Introduction and clinical picture
Androgenetic alopecia is one of the most common causes of hair loss worldwide. A progressive decline in the diameter, length, and pigmentation of the hair shaft with characteristic distribution is observed.
Male pattern hair loss (androgenetic alopecia)
This occurs when androgens induce miniaturisation through shortening of the anagen duration and prolongation of the telogen phase in genetically susceptible hair follicles. It is characterised by frontotemporal recessions and loss of hair over the vertex. Complete loss of hair can occur except at the lateral and posterior margins of the scalp.
Female pattern hair loss (FPHL)
This condition is a multifactorial disorder in which different genes, increased dihydrotestosterone production in the skin, lack of intracutaneous synthesised estrogens, and abnormalities in prolactin-mediated signalling may contribute to the pathogenesis. It is characterised by diffuse thinning without frontal hairline recession.
Trichoscopic features
Assessment of the scalp should be undertaken in the midline of the frontal area at a point 2cm from the frontal hair and compared with the occipital area of scalp.
Diagnostic signs:
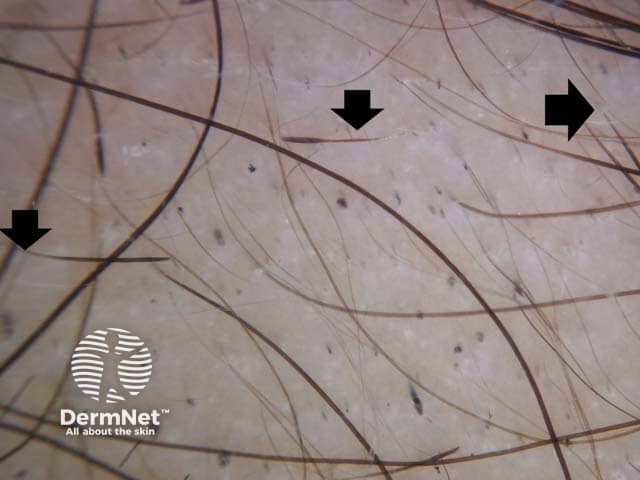
- Hair shaft thickness diversity (anisotrichosis): a diversity ≥20% is diagnostic of androgenetic alopecia
- Reduced number of triple hairs and increased number of single hairs per follicular unit in the mid-frontal area compared to the occipital area.
Other signs:
- Thin hairs: detection of >7 thin, short, regrowing hairs in the frontal area with 20x magnification suggests early-stage female pattern hair.
- Yellow dots, pinpoint white dots, focal atrichia, and scalp pigmentation (white peripilar sign) are detected in advanced stages of the disease, while brown peripilar pigmentation is a sign of early disease.

Dermoscopic image of androgenetic alopecia in a male patient showing hair shaft diversity of more than 20%. (MPHL-patient1)
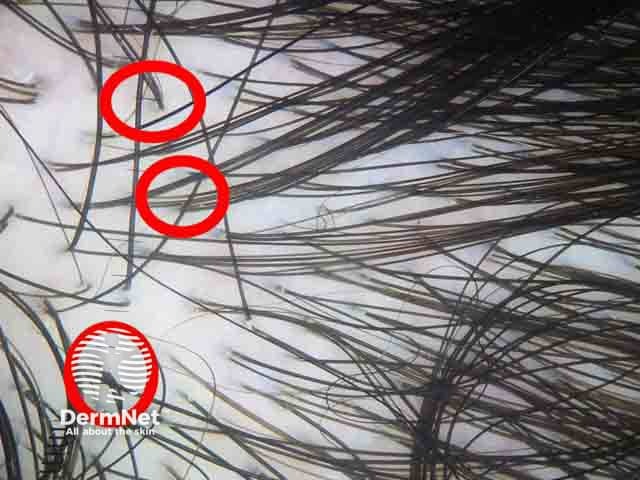
Dermoscopic image showing reduced number of triple hairs (red circles) in the mid-frontal area compared to the occipital area denoting female pattern hair loss. (FPHL-patient1)
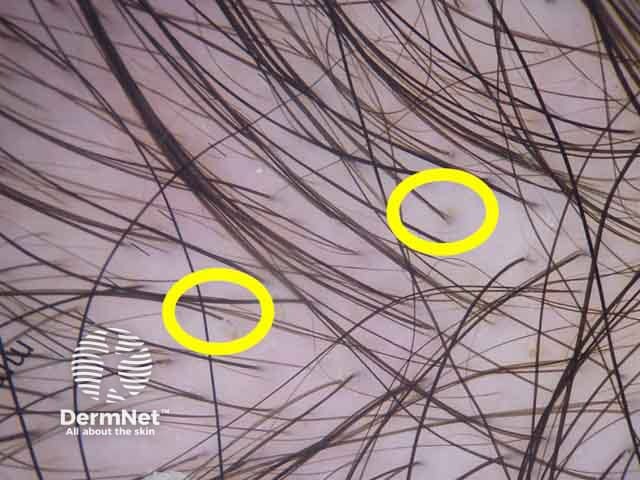
Dermoscopic image showing increased number of single hairs per follicular unit (yellow circles) in the mid-frontal area compared to the occipital area denoting female pattern hair loss. (FPHL-patient1)
Alopecia areata
Introduction and clinical picture
Alopecia areata is a chronic inflammatory T-cell mediated autoimmune disease targeting the hair follicles of the scalp and body. Clinical subtypes include:
- Patchy
- Alopecia totalis, universalis
- Ophiasis.
Associated nail changes include fine pitting, longitudinal ridges, and thinning may be observed.
Trichoscopic features
Trichoscopic features of alopecia areata differ according to activity, severity, and duration of disease.
Signs of active disease:
- Black dots (cadaverous hairs)
- Micro–exclamation mark hairs.
Signs of severe long-standing disease:
- Honeycomb pattern pigmentation
- Cumulus-like clustered white dots
- White dots.
Other signs:
- Tapered hairs: pathognomonic sign of alopecia areata
- Yellow dots:
- Observed in all stages of the disease however are considered a sign of severe condition
- Non-specific for alopecia areata as they are detected in telogen effluvium and trichotillomania.
- Broken hairs: observed in patchy alopecia areata patients
- Regrowing upright or circle hairs
- Short vellus hairs are commonly observed in alopecia universalis patients with remitting disease pattern.
- Hidden hairs in which a whitish grey veil covers their proximal end.
- Coudability sign is described as kinking of terminal hair towards its proximal ends when pushed perpendicular to the skin. They may represent a sign of disease activity.
- Thin arborising vessels
- ‘i hair sign’ is described as short hair with accentuated distal end, resembling the letter (i). This sign is considered a positive prognostic marker in patients with alopecia areata and trichotillomania as well.
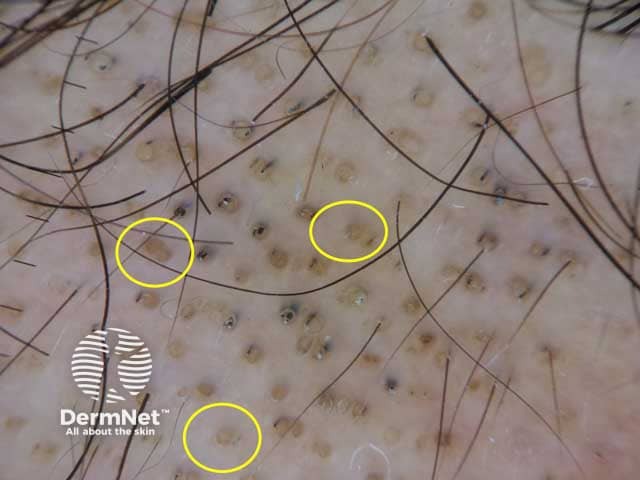
Dermoscopic image of alopecia areata showing yellow dots; follicular infundibula filled with keratinous material with no hair shafts. Black dots are also presented. (AA-patient2)
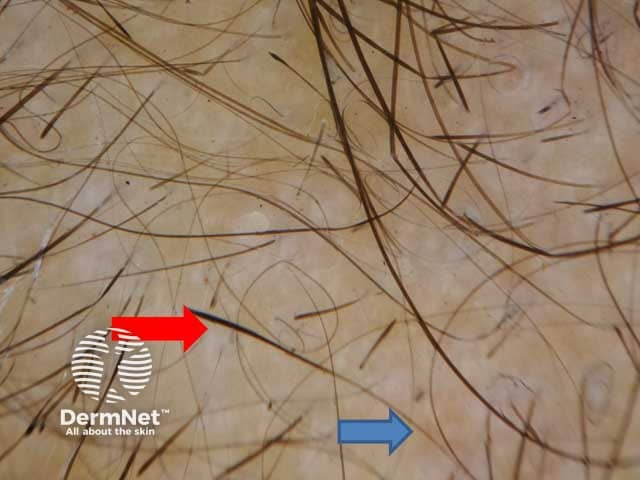
Thinning of the hair shaft at the proximal end (blue arrow) with normal thickness at the distal end (red arrow)

Dermoscopic image of alopecia areata presenting with exclamation mark hairs

Dermoscopic image of alopecia areata showing a pigtail hair: short twisted hair representing a regrowing hair
Dermoscopic image of a male patient with alopecia areata showing multiple exclamation mark hairs (denoted by black arrows)
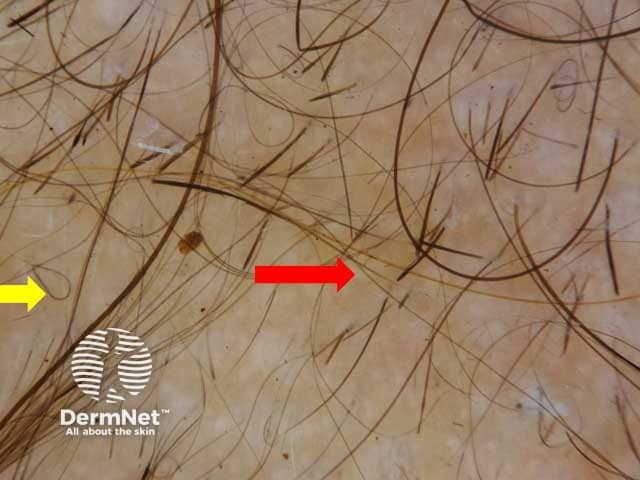
Dermoscopic image of a male patient with alopecia areata showing tapered hair (Red arrow) and regrowing hair (Yellow arrow)
Diffuse alopecia
Introduction and clinical picture
Diffuse alopecia (alopecia areata incognito) is a variant of alopecia areata, characterised by diffuse hair thinning with an absence of the typical patches of alopecia. It is more evident in the occipital and parietal regions and usually affects adult females. The diagnosis is confirmed only by histopathology as trichoscopic features are not specific.
Trichoscopic features
- Numerous uniform yellow dots.
- Short re-growing hairs.
- Yellow dots with vellus hairs.
- Pigtail hairs.
Telogen effluvium
Introduction and clinical picture
Telogen effluvium is characterised by excessive shedding of hair in the telogen phase. Alteration of the normal hair cycle occurs as a result of psychological and emotional stress. In scalp hair, more than 20% telogen hairs is considered diagnostic. Clinically, telogen effluvium may be:
Acute type
Often occurs 3 months after the triggering event such as high fever, surgical trauma, sudden starvation, and haemorrhage. However, in one-third of patients with telogen effluvium, no triggering event is identified.
Chronic type
Hair shedding persists for more than 6 months. It occurs due to chronic primary telogen effluvium, or due to underlying medical disorder, eg. thyroid disease, iron deficiency anaemia, acrodermatitis enteropathica, and malnutrition.
Trichoscopic features
The role of trichoscopy in diagnosis of telogen effluvium is limited. Trichoscopic features are not specific and include:
- The presence of yellow dots representing the empty follicles.
- Upright re-growing hairs.
- Lack of features of any other disease.
- The findings are described in the entire scalp; hence help to differentiate telogen effluvium from androgenetic alopecia.

Clinical image of a female patient with diffuse shedding of hair. (TE-patient1)
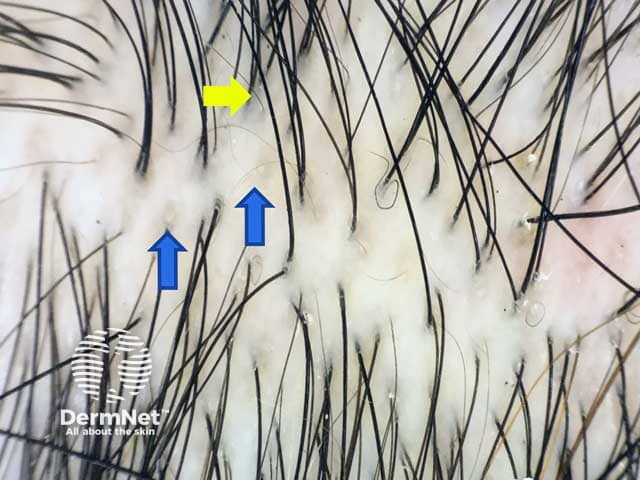
Dermoscopic image showing yellow dots representing the empty follicles (blue arrows) and upright re-growing hairs (yellow arrow) all over the scalp denoting telogen effluvium. (TE-patient1)
Anagen effluvium
Introduction and clinical picture
Anagen effluvium is a diffuse loss of hair in the anagen phase. It occurs in patients undergoing chemotherapy, or radiation therapy due to alteration of the hair cycle.
Trichoscopic features
- Monilethrix-like hairs.
- Black dots.
- Flame hairs.
- Yellow dots.
- Tapered fractured hair.
- Pohl pinkus.
Tractional alopecia
Introduction and clinical picture
Tractional alopecia is a form of traumatic hair loss, due to severe tension on scalp hairs. Frontal and tempro-parietal areas are most frequently affected. It may be marginal or non-marginal. The marginal type shows mild perifollicular erythema in areas of traction. This type is common in children and women of African descent. Non-marginal type is quite common in neonates affecting the occipital area within the first weeks of life.
Trichoscopic features
The main trichoscopic clues for diagnosis are:
- Reduced hair density
- Vellus hairs
- Broken hairs
- Short regrowing hairs
- Hair casts at the periphery of the lesion denoting continuous traction.
- Fringe sign - the appearance of vellus hairs retained at the edge of the affected area in marginal-type tractional alopecia.
- Brown outlined follicular openings with absence of hairs
- Irregular small white dots
- Yellow dots
- Extravasated blood.

Clinical picture of a female patient with patchy hair loss in the temporal area. (TA-patient1)
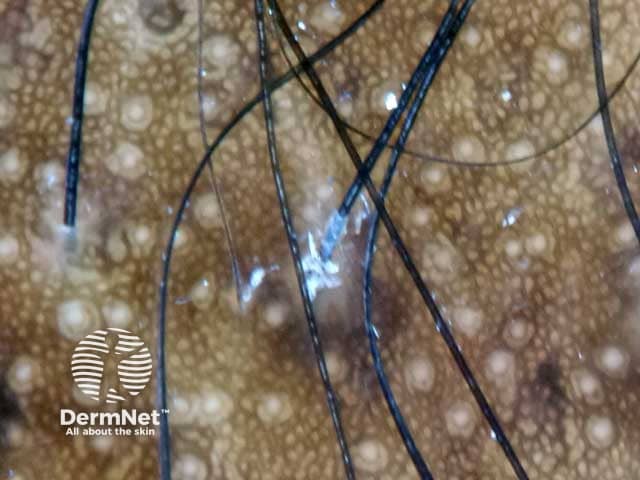
Dermoscopic image of hair cast represented by detached hyperkeratotic and parakeratotic cells of the inner root sheath
For general information on features found using trichoscopy, see trichoscopy (an overview).
Bibliography
- Al-Refu K. Clinical Significance of Trichoscopy in Common Causes of Hair Loss in Children: Analysis of 134 Cases. Int J Trichology. 2018;10(4):154-161. doi:10.4103/ijt.ijt_101_17. Journal
- Alessandrini A, Starace M, Bruni F, et al. Alopecia Areata Incognita and Diffuse Alopecia Areata: Clinical, Trichoscopic, Histopathological, and Therapeutic Features of a 5-Year Study [published correction appears in Dermatol Pract Concept. 2019 Dec 31;10(1):e2020027]. Dermatol Pract Concept. 2019;9(4):272–7. Published 2019 Oct 31. doi:10.5826/dpc.0904a05. Journal
- Bapu NG, Chandrashekar L, Munisamy M, Thappa DM, Mohanan S. Dermoscopic findings of alopecia areata in dark skinned individuals: an analysis of 116 cases. Int J Trichology. 2014;6(4):156-159. doi:10.4103/0974-7753.142853. Journal
- Billero V, Miteva M. Traction alopecia: the root of the problem. Clin Cosmet Investig Dermatol. 2018;11:149–59. Published 2018 Apr 6. doi:10.2147/CCID.S137296. Journal
- Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008;47(7):688-693. doi:10.1111/j.1365-4632.2008.03692.x. Journal
- Jain N, Doshi B, Khopkar U. Trichoscopy in alopecias: diagnosis simplified. Int J Trichology. 2013;5(4):170-178. doi:10.4103/0974-7753.130385. Journal
- Mahmoudi H, Salehi M, Moghadas S, Ghandi N, Teimourpour A, Daneshpazhooh M. Dermoscopic Findings in 126 Patients with Alopecia Areata: A Cross-Sectional Study. Int J Trichology. 2018;10(3):118-123. doi:10.4103/ijt.ijt_102_17. Journal
- Miteva M, Tosti A. Flame Hair. Skin Appendage Disord. 2015;1(2):105–9. doi:10.1159/000438995. Journal
- Rakowska A, Maj M, Zadurska M, et al. Trichoscopy of Focal Alopecia in Children - New Trichoscopic Findings: Hair Bulbs Arranged Radially along Hair-Bearing Margins in Aplasia Cutis Congenita. Skin Appendage Disord. 2016;2(1-2):1-6. doi:10.1159/000445721. Journal
- Rebora A. Telogen effluvium: a comprehensive review. Clin Cosmet Investig Dermatol. 2019;12:583-590. Published 2019 Aug 21. doi:10.2147/CCID.S200471. Journal
- Tosti A, Whiting D, Iorizzo M, et al. The role of scalp dermoscopy in the diagnosis of alopecia areata incognita. J Am Acad Dermatol. 2008;59(1):64-67. doi:10.1016/j.jaad.2008.03.031. Journal
On DermNet
- Trichoscopy overview
- Trichoscopy of inflammatory conditions
- Trichoscopy of scalp infestations
- Trichoscopy of localised noncicatricial hair loss
- Androgenetic areata
- Alopecia areata
- Alopecia areata/ Diffuse alopecia
- Telogen effluvium
- Anagen effluvium
- Tractional alopecia
