Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Female pattern hair loss — extra information
Female pattern hair loss
Author: Dr Leona Yip, Research Fellow, St Vincent's Hospital, Melbourne, Australia, 2007. Updated by Prof Rod Sinclair, Melbourne, Australia, July 2015.
Images courtesy of R. Sinclair, FACD
Introduction Causes Introduction - normal hair growth cycle Hair shedding Hair miniaturisation Progression Effects Hormone tests Treatment Where to seek help
What is female pattern hair loss?
Female pattern hair loss (FPHL) is a distinctive form of diffuse hair loss that occurs in women with androgenetic alopecia. Many women are affected by FPHL. Around 40% of women by age 50 show signs of hair loss and less than 45% of women reach the age of 80 with a full head of hair.
In FPHL, there is diffuse thinning of hair on the scalp due to increased hair shedding or a reduction in hair volume, or both. It is normal to lose up to 50-100 hairs a day. Another condition called chronic telogen effluvium also presents with increased hair shedding and is often confused with FPHL. It is important to differentiate between these conditions as management for both conditions differ.
FPHL presents quite differently from the more easily recognisable male pattern baldness, which usually begins with a receding frontal hairline that progresses to a bald patch on top of the head. It is very uncommon for women to bald following the male pattern unless there is excessive production of androgens in the body.





Grade 5
What causes female pattern hair loss?
FPHL has a strong genetic predisposition. The mode of inheritance is polygenic, indicating that there are many genes that contribute to FPHL, and these genes could be inherited from either parent or both. Genetic testing to assess the risk of balding is currently not recommended, as it is unreliable.
Currently, it is not clear if androgens (male sex hormones) play a role in FPHL, although androgens have a clear role in male pattern baldness. The majority of women with FPHL have normal levels of androgens in their bloodstream. Due to this uncertain relationship, the term FPHL is preferred to ‘female androgenetic alopecia’.
The role of oestrogen is uncertain. FPHL is more common after the menopause suggesting oestrogens may be stimulatory for hair growth. But laboratory experiments have also suggested oestrogens may suppress hair growth.
What is the normal hair growth cycle?
Everyone is born with a fixed number of hair follicles on the scalp that produce hairs throughout life. Hair grows from the base of the follicle at a rate of about one centimetre a month for about three years. This growth phase is called anagen. After anagen, the hair dies (catagen hair) and no longer grows. It sits dormant in the follicle for a three-month phase called telogen. After telogen, the hair follicle undergoes another anagen phase to produce new hair that grows out of the same follicle. As it grows, the old telogen hair is dislodged or pushed out. The hair cycle continues throughout life.
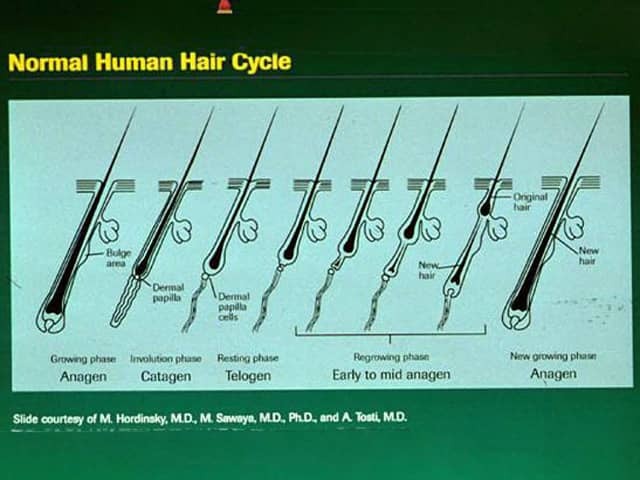
Hair cycle
Image © 1998 Merck Sharpe and Dohme (with permission)
Hair shedding
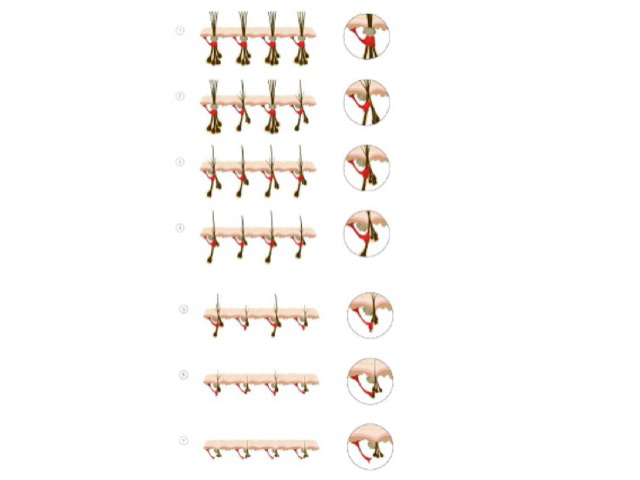
Increased hair shedding or telogen effluvium is a feature to FPHL. Women can use the hair shedding guide below to define whether hair shedding is normal or excessive,
To assess hair shedding, women should choose which of the six photographs of hair bundles best represents how much hair they shed on an average day.
Doctors can use the hair shedding scale to score hair loss at each patient visit to assess response to treatment. It can also be used in clinical trials to assess new treatments for excess hair shedding.
Hair shedding guide
Baseline shedding scores |
Example images |
|---|---|
Normal (1 to 3) |



|
Borderline (4) |

|
Excessive (5 - 6) |


|
Images courtesy of R. Sinclair, FACD
Hair miniaturisation
Unlike other areas of the body, hairs on the scalp to grow in tufts of 3–4. In androgenetic alopecia, the tufts progressively lose hairs. Eventually, when all the hairs in the tuft are gone, bald scalp appears between the hairs.
Hair miniaturisation
How long does it take for FPHL to progress?
FPHL can affect women in any age group, but it occurs more commonly after menopause. The hair loss process is not constant and usually occurs in fits and bursts. It is not uncommon to have accelerated phases of hair loss for 3–6 months, followed by periods of stability lasting 6–18 months. Without medication, it tends to progress in severity over the next few decades of life.
What are the effects of female pattern hair loss?
Many studies have shown that hair loss is not merely a cosmetic issue, but it also causes significant psychological distress. Compared to unaffected women, those affected have a more negative body image and are less able to cope with daily functioning. Hair loss can be associated with low self-esteem, depression, introversion, and feelings of unattractiveness. It is especially hard to live in a society that places great value on youthful appearance and attractiveness.
Should I have any hormone tests done?
Blood tests include female and male sex hormone levels as well as thyroid function, as part of the diagnostic workup.
The majority of women affected by FPHL do not have underlying hormonal abnormalities. However, a few women with FPHL are found to have excessive levels of androgens. These women also tend to suffer from acne, irregular menses and excessive facial and body hair. These symptoms are characteristic of the polycystic ovarian syndrome (PCOS) although the majority of women with PCOS do not experience hair loss. Less often, congenital adrenal hyperplasia may be responsible.
What treatments are available?
Treatments are available for FPHL although there is no cure. It is important to manage expectations when seeking treatment, as the aim is to slow or stop the progression of hair loss rather than to promote hair regrowth. However, some women do experience hair regrowth with treatment. Results are variable, and it is not possible to predict who may or may not benefit from treatment.
A Cochrane systematic review published in 2012 concluded that minoxidil solution was effective for FPHL. Minoxidil is available as 2% and 5% solutions; the stronger preparation is more likely to irritate and may cause undesirable hair growth unintentionally on areas other than the scalp.
Hormonal treatment, i.e. oral medications that block the effects of androgens (e.g. spironolactone, cyproterone, finasteride and flutamide) is also often tried.
A combination of low dose oral minoxidil (eg, 2.5 mg daily) and spironolactone (25 mg daily) has been shown to significantly improve hair growth, reduce shedding and improve hair density.
Once started, treatment needs to continue for at least six months before the benefits can be assessed, and it is important not to stop treatment without discussing it with your doctor first. Long term treatment is usually necessary to sustain the benefits.
Cosmetic camouflages include coloured hair sprays to cover thinning areas on the scalp, hair bulking fibre powder, and hair wigs. Hair transplantation for FPHL is becoming more popular although not everyone is suitable for this procedure.
Low-level laser therapy is of unproven benefit in pattern balding, but one device has been approved by the FDA for marketing. Platelet-rich plasma injections are also under investigation. Further studies are required to determine the magnitude of the benefit if any.
Where do I go to seek help?
Your first stop would be to see your general practitioner (GP) who can perform a medical workup to exclude other reasons for hair loss. Your GP can refer you to a dermatologist for further management of FPHL. Sometimes, it may be necessary for your doctor to perform a scalp biopsy to confirm this diagnosis.
It is important to seek reliable information and advice from authoritative sources as there are many bogus treatments that are expensive and do not work.
References
- Gan D, Sinclair R. Prevalence of male and female pattern hair loss in Maryborough. J Investig Dermatol Symp Proc 10(3), 184-9 (2005). Journal
- The Australasian Hair and Wool Research Society patient information leaflet on Understanding androgenetic hair loss in women (2000).
- Yip L, Sinclair R. Antiandrogen therapy for androgenetic alopecia. Expert Rev Dermatol 1(2):261–9 (2006). PubMed
- Bad Hair Day by Francesca Collins, Sebastiana Bondo and Rodney Sinclair. Lothian Books, 2006 (highly recommended read for patients).
- Sinclair R, Patel M, Dawson TL, Yazdabadi A, Yip L, Perez A, Rufaut NW. Hair loss in women: medical and cosmetic approaches to increase scalp hair fullness. Br J Dermatol 2011; 165: 12-18. PubMed
- van Zuuren EJ, Fedorowicz Z, Carter B. Evidence-based treatments for female pattern hair loss: a summary of a Cochrane systematic review. Br J Dermatol 2012:167;995–1010. PubMed
- Sinclair RD. Female pattern hair loss: a pilot study investigating combination therapy with low-dose oral minoxidil and spironolactone. Int J Dermatol. 2017 Dec 12. doi: 10.1111/ijd.13838. [Epub ahead of print] PubMed PMID: 29231239. PubMed.
- Olamiju, Brianna et al. Combination oral minoxidil and spironolactone for the treatment of androgenetic alopecia in adolescent girls Journal of the American Academy of Dermatology, Volume 84, Issue 6, 1689–1691; June 2021. Journal
On DermNet
- Hair loss
- Diffuse alopecia
- Male pattern hair loss
- Alopecia areata
- Telogen Effluvium
- Alopecia from drugs
- Minoxidil
- Hormonal treatment
- Low-level laser therapy for hair loss
- Psychological effects of hair loss
Other websites
- Androgenetic Alopecia — Medscape Reference
- Patient information: Hair loss in men and women (The Basics) — UpToDate
- Patient information: Hair loss in men and women (androgenetic alopecia) (Beyond the Basics) — UpToDate (for subscribers)
