Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Pyogenic granuloma — extra information
Pyogenic granuloma
Authors: Vanessa Ngan, Staff Writer, 2003. Updated by Dr Malini Sivasaththivel, RMO, Eastern Health, Box Hill, Australia; Dr Smriti Tandon, Dermatology Registrar, Eastern Health, Box Hill, Australia; Dr Lena Ly, Dermatologist, Eastern Health, Box Hill, Australia. Copy edited by Gus Mitchell. January 2021.
Introduction
Demographics
Causes
Clinical features
Dermoscopic features
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
What is a pyogenic granuloma?
Pyogenic granuloma is an acquired benign proliferation of capillary blood vessels of the skin and oral cavity. The name is a misnomer as it is a form of lobular capillary haemangioma, not due to infection. Pyogenic granuloma has many synonyms including granuloma gravidarum or pregnancy tumour when occurring in pregnancy.

Pyogenic granuloma

Pyogenic granuloma

Pyogenic granuloma
Who gets pyogenic granuloma?
Pyogenic granuloma often occurs in children around 6 years of age and during teenage and young adult life. There is an overall male predominance (3:2) except for oral lesions due to their association with pregnancy and oral contraceptive use. There is no racial predilection.
What causes pyogenic granuloma?
Factors associated with the development of a pyogenic granuloma may include:
- Trauma — recent minor trauma accounts for 7% of presentations and, in the oral cavity, chronic minor irritation is thought to be a common trigger. Nasal piercings are reported in association with intranasal pyogenic granuloma.
- Hormonal influences — can occur with oral contraceptive use and in 5% of pregnancies.
- Medications — oral retinoids, protease inhibitors (used in the treatment of HIV/AIDS), targeted cancer therapies, and immunosuppression.
- Infection — Staphylococcus aureus is frequently detected. In the oral cavity, poor dental hygiene is a common association. There is no evidence for a viral aetiology.
What are the clinical features of pyogenic granuloma?
Pyogenic granuloma of the skin presents as a painless red fleshy nodule, typically 5-10mm in diameter, that grows rapidly over a few weeks. The surface is initially smooth but can ulcerate, become crusty, or verrucous. Pyogenic granuloma is usually solitary, but multiple nodules and satellite lesions can erupt. The most common sites involved are the fingers and face. Pyogenic granuloma easily bleeds with minor trauma.
Oral mucosal pyogenic granulomas typically develop on the lip and gums (gingiva) as pedunculated or sessile slow-growing painless red papules ranging in size from a few millimetres to several centimetres. The surface can be ulcerated with a yellow-fibrinous surface, and easy bleeding. With time, the lesion becomes a paler pink colour. Other mucosal sites that can be affected include the conjunctiva and nasal mucosa.




New lesion

2 weeks later

4 weeks after first photograph
What are the dermoscopic features of pyogenic granuloma?
Pyogenic granuloma has a distinct keratinised border forming a white collarette. Vascular structures are usually present and there are red homogenous areas with no clear lacunar pattern. White linear ‘rail lines’ are an important feature.
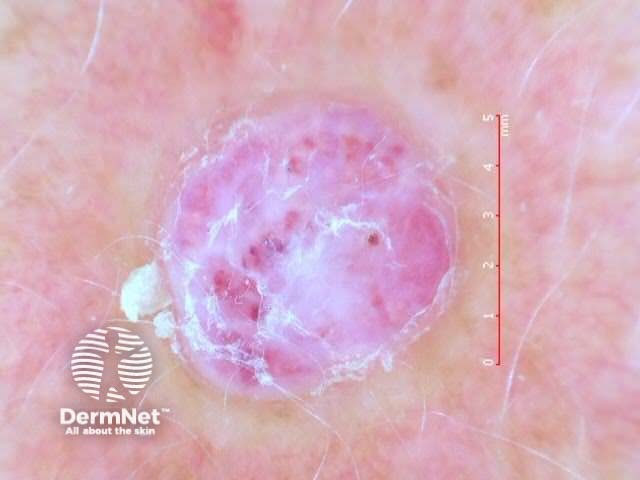
Pyogenic granuloma dermoscopy
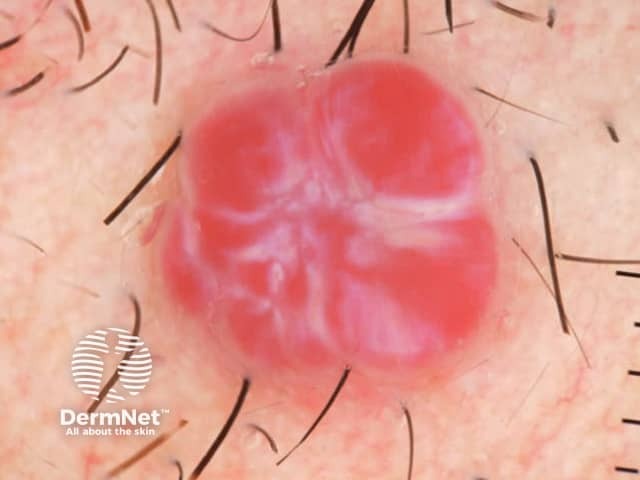
Red clods separated by white lines in pyogenic granuloma
What are the complications of pyogenic granuloma?
Pyogenic granuloma can bleed profusely and frequently with minor trauma, resulting in anaemia.
Oral pyogenic granuloma can rarely cause significant bone loss.
How is pyogenic granuloma diagnosed?
Pyogenic granuloma is usually a clinical diagnosis. However, tissue may be submitted for histology following surgical treatment of the lesion or where there are concerns about the diagnosis.
Histology of pyogenic granuloma shows a prominent lobular capillary arrangement in the dermis. The overlying epidermis may be thinned or ulcerated, and the peripheral collarette is formed by elongated rete ridges and eccrine ducts. Inflammatory changes and signs of haemorrhage are secondary.

Dermal lobular arrangement of capillaries
There are two distinct histological types of oral pyogenic granuloma. In addition to the lobular capillary haemangioma pattern, a second type shows a distinct granulation tissue-like vascular proliferation which is postulated to have a different aetiology and evolution.
What is the differential diagnosis for pyogenic granuloma?
The clinical differential diagnosis of cutaneous pyogenic granuloma includes:
Amelanotic or hypomelanotic melanoma is the most important differential diagnosis even on dermoscopy with many shared features.
The differential diagnosis of oral cavity pyogenic granuloma includes the above, as well as the site-specific peripheral giant cell granuloma and peripheral ossifying fibroma.
The differential diagnosis on histology includes cherry angioma and bacillary angiomatosis.
What is the treatment for pyogenic granuloma?
General measures
Treating or removing triggering factors is important to minimise the risk of recurrence. This may include:
- Ceasing drug triggers
- Careful oral hygiene
- Dental treatment of oral trauma caused by teeth
- Removal of adjacent piercings.
Topical treatment of pyogenic granuloma
- Imiquimod cream 5%
- Timolol gel 0.5% and other topical (or oral) beta-blockers
- Intralesional steroid injection
- Cryotherapy
- Table salt therapy — table salt is applied under occlusion after protecting the surrounding skin with yellow soft paraffin.
Procedural treatment of pyogenic granuloma
- Curettage and cautery
- Surgical excision
- Vascular and ablative lasers
What is the outcome for pyogenic granuloma?
Pyogenic granuloma rarely resolves spontaneously except post-partum for lesions associated with pregnancy. Recurrence is common, especially for gingival lesions, after inadequate treatment or persistent aetiological factors.
Bibliography
- Calonje E. Soft tissue tumours and tumour-like conditions. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D (eds). Rook’s Textbook of Dermatology, 9th edn. Wiley Blackwell, 2016: 137.26–8.
- Daruwalla SB, Ghate S, Dhurat R. Establishing the efficacy and safety of the novel use of common salt for the treatment of pyogenic granuloma. Clin Exp Dermatol. 2021;46(7):1243-1247. doi:10.1111/ced.14658 Journal
- Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48(4):167–75. doi:10.2334/josnusd.48.167. PubMed
- Patterson JW. Weedon’s Skin Pathology, 5th edn. Elsevier, 2020: p1144–5.
- Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. Int J Dermatol. 2019;58(6):642–8. doi:10.1111/ijd.14268. PubMed
- Zaballos P, Carulla M, Ozdemir F, et al. Dermoscopy of pyogenic granuloma: a morphological study. Br J Dermatol. 2010;163(6):1229–37. doi:10.1111/j.1365-2133.2010.10040.x. PubMed
On DermNet
- Bacillary angiomatosis pathology
- Cherry angioma pathology
- Dermal and subcutaneous lesions
- Dermatoscopy of other non-melanocytic lesions
- Pulsed dye laser treatment
Other websites
- Dermatologic Manifestations of Pyogenic Granuloma (Lobular Capillary Hemangioma) — Medscape Drugs & Diseases
- Pyogenic Granuloma — British Association of Dermatologists
