Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lichen planus — extra information
Lichen planus
Author(s): Dr Jacqueline Chen, General Practitioner, Australia (2022); Prof Amanda Oakley, Dermatologist, New Zealand (2015); minor update by Dr Jing Liu, Resident Medical Officer, Australia (2023)
Reviewing dermatologist: Dr Ian Coulson (2023)
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
What is lichen planus?
Lichen planus (LP) is a chronic inflammatory condition affecting the skin and mucosal surfaces. There are several clinical types:
- Cutaneous lichen planus
- Mucosal lichen planus
- Lichen planopilaris
- Lichen planus of the nails
- Lichen planus pigmentosus
- Lichenoid drug eruption.
Click here for images of lichen planus
Who gets lichen planus?
Lichen planus affects approximately 1% of the population worldwide, mostly affecting adults aged between 30 to 60 years. It has no strong racial predilection.
Approximately 10% of those affected have lichen planus of the nails while half of those affected have oral lichen planus, which is more common in women than in men.
What causes lichen planus?
Lichen planus is a T-cell mediated autoimmune disorder in which inflammatory cells attack an unknown protein within the skin and mucosal keratinocytes.
Contributing factors to lichen planus may include:
- Genetic predisposition
- Physical and emotional stress
- Injury to the skin; lichen planus often appears where the skin has been scratched or after surgery (koebnerisation)
- Localised skin disease such as herpes zoster
- Systemic viral infection, such as hepatitis C (which might modify self-antigens on the surface of basal keratinocytes)
- Contact allergy, such as to metal fillings in oral lichen planus (rare) and colour photographic developers
- Drugs; gold, quinine, quinidine, and others can cause a lichenoid rash.
Lichenoid inflammation is also notable in graft-versus-host disease.
Vitamin D deficiency may be associated with oral lichen planus. Its association with other types of LP remains unexplored.
What are the clinical features of lichen planus?
Lichen planus may cause a small number or many lesions on the skin and mucosal surfaces.
Cutaneous lichen planus
The usual presentation of the disease is classical lichen planus. Symptoms can range from none (uncommon) to intense itch.
- Papules and polygonal plaques are shiny, flat-topped, and firm on palpation.
- The plaques are crossed by fine white lines called Wickham striae.
- Hypertrophic lichen planus can be a scaly and pruritic rash.
- Atrophic lichen planus is a rare annular variant with an atrophic centre.
- Annular lichen planus describes the development of violaceous plaques with central clearing often involving penis, scrotum, and intertriginous areas.
- Size ranges from pinpoint to larger than a centimetre.
- Distribution may be scattered, clustered, linear, annular, or actinic (sun-exposed sites such as face, neck, and backs of the hands).
- Location can be anywhere, but most often front of the wrists, lower back, and ankles.
- Colour depends on the patient’s skin type. New papules and plaques often have a purple or violet hue, except on palms and soles where they are yellowish-brown.
- Plaques resolve after some months to leave greyish-brown post-inflammatory macules that can take a year or longer to fade.

Papular lichen planus coalescing into plaques on the wrist (PLP-patient1)

Flat topped, shiny, polygonal papules of lichen planus on the volar wrist (PLP-patient1)

A plaque of lichen planus showing Wickham striae

Papular lichen planus with Koebner phenomenum in skin of colour

Lichen planus over the ankle and heel

Papular lichen planus with a linear Koebner lesion due to a scratch
Click here for more images of cutaneous lichen planus
Oral lichen planus
The mouth is often the only affected area and often involves the inside of the cheeks and the sides of the tongue, but the gums and lips may also be involved.
The most common patterns are:
- Painless white streaks in a lacy or fern-like pattern (Wickham striae)
- Painful and persistent erosions and ulcers (erosive LP)
- Diffuse redness and peeling of the gums (desquamative gingivitis)
- Localised inflammation of the gums adjacent to amalgam fillings.
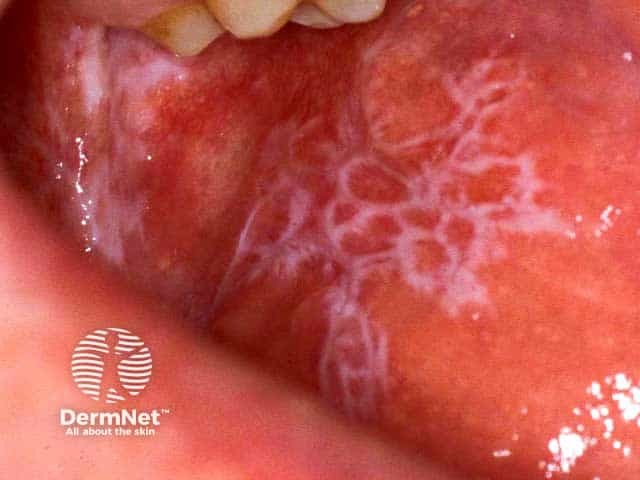
Reticulate buccal mucosal lichen planus

Lacy reticulated lichen planus covering the entire tongue

Erosive lichen planus on the lateral border of the tongue

Reticulate and violaceous lichen planus on the lower lip

Reticulate and eroded lichen planus on the lower lip
Click here for more images of oral lichen planus
Vulval lichen planus
Lichen planus may affect the labia majora, labia minora, and vaginal introitus. Presentation includes:
- Painless white streaks in a lacy or fern-like pattern
- Painful and persistent erosions and ulcers (erosive LP)
- Scarring, resulting in adhesions, resorption of labia minora and introital stenosis
- Painful desquamative vaginitis, preventing intercourse and causing a mucky vaginal discharge; the eroded vagina may bleed easily on contact
- Overlap with vulval lichen sclerosus that most commonly affects women over 50 years of age.
Click here for images of erosive vulval lichen planus
Penile lichen planus
- Classical papules in a ring around the glans.
- White streaks and erosive lichen planus may occur but are less common.
Click here for images of genital lichen planus
Other mucosal sites
Erosive lichen planus uncommonly affects the lacrimal glands, eyelids, external ear canal, oesophagus, larynx, bladder, and anus.
Lichen planopilaris
Lichen planopilaris presents as tiny red spiny follicular papules and extending smooth areas on the scalp or less often, elsewhere on the body. Rarely, blistering occurs in the lesions. Destruction of the hair follicles leads to permanently bald patches characterised by sparse 'lonely hairs'.
Frontal fibrosing alopecia is a form of lichen planopilaris that affects the anterior scalp, forehead, and eyebrows.
Pseudopelade of Brocq may be a variant of lichen planus without inflammation or scaling. Areas of scarring without hair slowly appear, described as looking 'like footprints in the snow'.

Lichen planopilaris
Nail lichen planus
- Lichen planus affects one or more nails, sometimes without involving the skin.
- It is called twenty-nail dystrophy if all nails are abnormal and nowhere else is affected.
- Lichen planus thins the nail plate, which may become grooved and ridged.
- The nail may darken, thicken or lift off the nail bed (onycholysis).
- Sometimes the cuticle is destroyed and forms a scar (pterygium).
- The nails may shed or stop growing altogether, and rarely, completely disappear (anonychia).

Complete nail plate destruction due to lichen planus

Ridging and roughness (onychorrhexis) of the finger nail plates due to nail unit lichen planus

Nail plate atrophy and destruction and pterygium development in nail unit lichen planus. Lichen planus is evident over the adjacent distal phalanx
Click here for more images of nail lichen planus
Lichen planus pigmentosus
- Characterised by ill-defined oval, greyish brown marks on the face and neck or trunk and limbs without an inflammatory phase.
- It is a form of acquired dermal macular hyperpigmentation.
- Can be provoked by sun exposure, but it can also arise in sun-protected sites such as the armpits.
- Diffuse, reticulate, and diffuse patterns.
- Similar to erythema dyschromicum perstans and might be the same disease.
- Rarely affects the lips, resulting in a patchy dark pigmentation on upper and lower lips.

Lichen planus pigmentosus of face

Lichen planus pigmentosus of lower back

Lichen planus pigmentosus of lower lip
Lichen planus actinicus (LPA)
- Other names include lichen planus subtropicus, lichen planus tropicus, lichenoid melanodermatitis, and summertime actinic lichenoid eruptions.
- Mainly occurs in young adults of Middle Eastern, East African, or Indian descent.
- Appears to be triggered by sunlight exposure (ie, photosensitive).
- Lesions typically:
- Involve sun-exposed area such as the forehead, cheeks, lips, neck, back of the hands, and forearms
- Worsen in summer and improve in winter
- Appear as red-brown annular plaques, or hyperpigmented patches.
- Lesions typically do not:
- Itch
- Involve the mucous membranes
- Display the Koebner phenomenon.
- Photosensitive lesions that appear whitish (dyschromic) pinhead and papules are called actinic lichen nitidus, which is now considered a separate and distinct entity from LPA.
- LPA is usually diagnosed based on lesion distribution and skin biopsy results.
Lichenoid drug eruption
- Lichenoid drug eruption refers to a lichen planus-like rash caused by medications.
- Asymptomatic or itchy; pink, brown, or purple; flat, slightly scaly patches most often arise on the trunk. The oral mucosa (oral lichenoid reaction) and other sites are also sometimes affected.
- Many drugs can rarely cause lichenoid eruptions. The most common are:
- Gold
- Hydroxychloroquine
- Captopril.
Quinine and thiazide diuretics cause a photosensitive lichenoid drug eruption.
Bullous lichen planus and lichen planus pemphigoides
Bullous lichen planus
- Produces blisters due to destruction of basal keratinocytes, and is rare.
Lichen planus pemphigoides
- Rare combination of lichen planus and bullous pemphigoid.
- Destruction of the basal keratinocytes exposes bullous pemphigoid antigen at the dermoepidermal junction (termed epitope spreading), followed by the development of circulating antibodies against BP antigen.
- Erythema and blisters develop both at the sites of and distant from lesions of lichen planus.

Severe lichen planus on the foot producing blisters (BLP-patient1)
How do clinical features vary in differing types of skin?
Hypertrophic, actinic variants, lichen planus pigmentosus, and residual post-inflammatory hyperpigmentation are more common amongst darker-skinned individuals.
What are the complications of lichen planus?
- Hypertrophic lichen planus may resemble squamous cell carcinoma. However, rarely, longstanding erosive lichen planus can result in true squamous cell carcinoma, most often in the mouth, vulva, or penis. This should be suspected if there is an enlarging nodule or an ulcer with thickened edges.
- Cancer is more common in smokers, those with a history of cancer in mucosal sites, and those who carry sexually acquired and oncogenic human papillomavirus.
- Oesophageal lichen planus can cause dysphagia, strictures, and possibly squamous cell carcinoma.
- Cancer from other forms of lichen planus is rare.
How is lichen planus diagnosed?
Lichen planus is diagnosed clinically in most cases. A skin biopsy is often recommended to confirm the diagnosis and to look for cancer. The histopathological signs are of a lichenoid tissue reaction affecting the epidermis.
Typical features include:
- Irregularly thickened epidermis
- Wedge-shaped hypergranulosis, ‘saw-tooth’ shaped rete ridges
- Civatte bodies (apoptotic keratinocytes) in the lower epidermis and upper dermis
- Liquefaction degeneration of the basal layer of the epidermis
- Band-like lymphocytic infiltrate at the dermo-epidermal junction.
Direct immunofluorescence studies are not routinely needed. Results may reveal colloid bodies in the papillary dermis with irregular deposits.
Patch testing may be recommended for patients with oral lichen planus affecting the gums and who have amalgam fillings, to assess for contact allergy to thiomersal (a mercurial compound) and other metals.
What is the differential diagnosis for lichen planus?
Differential diagnoses of lichen planus are broad and can be categorised into:
Table 1: Differential diagnoses for lichen planus
Papular classic |
|
Annular LP |
|
Linear |
|
Hypertrophic |
|
Lichen planus pigmentosus |
|
Lichen planus actinicus |
|
Vesicobullous |
|
Atrophic |
|
Vulval lichen planus |
|
Oral lichen planus |
|
Lichen planus of nails |
|
Lichen planopilaris |
What is the treatment for lichen planus?
General measures
- Avoid soaps and shower gels that will exacerbate scaling.
- Use emollients regularly.
- Sedating antihistamines may help troublesome nocturnal itch.
Specific treatment
Treatment is not always necessary as cutaneous LP can be self-limiting and treatment goals are to manage pruritus. Local treatments for the symptomatic cutaneous or mucosal disease are:
- Potent topical corticosteroids (including steroid impregnated tape)
- Topical calcineurin inhibitors, tacrolimus ointment, and pimecrolimus cream
- Topical retinoids
- Intralesional steroid injections.
Systemic treatment for widespread lichen planus or severe local disease often includes a 1- to 3-month course of systemic steroids (eg, prednisone), while commencing another agent from the following list:
Anecdotal success is reported from long courses of antibiotics e.g. metronidazole, sulfasalazine, antifungals (such as griseofulvin), and JAK inhibitors. Lichen planopilaris is reported to improve with pioglitazone and tetracyclines.
In lichen planus actinicus, phototherapy should be avoided because lesions are typically triggered by sun exposure. Sun protection, including use of sunscreen, is an essential component of treatment.
In oral lichen planus, limited evidence is found in using apremilast. Successful treatment of oral and cutaneous lichen planus with adalimumab has previously been reported. Tildrakizumab has been shown to demonstrate positive results in erosive oral lichen planus in an isolated case study.
In cases of oral lichen planus affecting the gums and buccal mucosa with contact allergy to mercury, the lichen planus may resolve on replacing the fillings with composite material. If the lichen planus is not due to mercury allergy, removing amalgam fillings is very unlikely to result in a cure.
For more information see, oral lichen planus and erosive lichen planus.
What is the outcome for lichen planus?
Lichen planus can have a chronic remitting and relapsing course. Cutaneous lichen planus tends to clear within a couple of years in most people, but post-inflammatory pigmentation may take years to subside.
Mucosal lichen planus is more likely to persist for a decade or longer. For lichen planopilaris, scarring is permanent, including scarring alopecia. Lichenoid drug eruption resolves slowly when the responsible medication is withdrawn.
Bibliography
- Le Cleach L, Chosidow O. Clinical practice. Lichen planus. N Engl J Med. 2012; 23;366(8):723–32. doi: 10.1056/NEJMcp1103641. Journal
- Gorouhi F, Davari P, Fazel N. Cutaneous and mucosal lichen planus: A comprehensive Review of clinical subtypes, risk factors, diagnosis and prognosis. Sci World J. 2014; 1–22. https://doi.org/10.1155/2014/742826. Journal
- Damsky W, Wang A, Olamiju B, Peterson D, Galan A, King B. Treatment of severe lichen planus with the JAK inhibitor tofacitinib. J Allergy Clin Immunol. 2020;145(6):1708–10.e2. doi: 10.1016/j.jaci.2020.01.031. Journal
- Ismail FF, Sinclair R. Clinical healing of erosive oral lichen planus with tildrakizumab implicates the interleukin-23/interleukin-17 pathway in the pathogenesis of lichen planus. Australas J Dermatol. 2020;61(2):244–5. doi: 10.1111/ajd.13183. Journal
- Motahari P, Pournaghi Azar F, Rasi A. Role of Vitamin D and Vitamin D Receptor in Oral Lichen Planus: A Systematic Review. Ethiop J Health Sci. 2020;30(4):615–622. doi: 10.4314/ejhs.v30i4.17. Article
- Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1(3):140–149. doi: 10.1016/j.ijwd.2015.04.001. Journal
On DermNet
- Oral lichen planus
- Lichen planus images
- Lichen planopilaris
- Frontal fibrosing alopecia
- Squamous cell carcinoma
- Lichenoid drug eruption
- Erosive lichen planus
- Drug eruptions
- Itchy skin lesions
- Genital skin problems
- Lichenoid disorders
- Direct immunofluorescence
- Acquired dermal macular hyperpigmentation
Other websites
- Spotlight on Red Scaly Rashes — DermNet e-lecture [Youtube]
- Lichen planus — The Australian College of Dermatologists
- Lichen planus — The Royal Women's Hospital, Victoria, Australia
- Steroid impregnated tape — YouTube: demonstrating tape application
- Vulvovaginal Disorders: A Pathway to Diagnosis and Treatment
