Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Pyoderma gangrenosum — extra information
Pyoderma gangrenosum
Authors: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1998. Updated September 2015. Further updated: Dr Gaurav Dhawan, Dermatology Specialty Trainee, Salford Royal Hospital United Kingdom. Copy edited by Gus Mitchell. March 2022
Introduction
Demographics
Causes
Clinical features
Diagnosis
Differential diagnoses
Treatment
Outlook
What is pyoderma gangrenosum?
Pyoderma gangrenosum (PG) presents as a rapidly enlarging, very painful ulcer. It is one of a group of autoinflammatory disorders known as neutrophilic dermatoses.
The name pyoderma gangrenosum is historical. The condition is not an infection (pyoderma), nor does it cause gangrene.
It is characterised by a full-thickness ulcer with blue/purple undermined borders and by pathergy.
Who gets pyoderma gangrenosum?
Pyoderma gangrenosum is a rare disease that affects males and females of any age but is more common in those aged over 50 years. It frequently is associated with an internal disease or condition. Its known associations include:
- Inflammatory bowel disease (ulcerative colitis and Crohn disease)
- Rheumatoid arthritis
- Myeloid blood dyscrasias including leukaemia
- Monoclonal gammopathy (usually IgA)
- Chronic active hepatitis
- Granulomatosis with polyangiitis
- PAPA syndrome
- Behçet disease
- Use of levamisole-adulterated cocaine
- Miscellaneous less-common associations.
About half of those affected by pyoderma gangrenosum have none of the associated risk factors.
Pyoderma gangrenosum associated with inflammatory bowel disease
IBD-associated pyoderma gangrenosum has the following characteristics:
- Pyoderma gangrenosum represents the second-most common cutaneous manifestation of IBD (1–3%).
- It is more commonly a complication of ulcerative colitis compared to Crohn disease.
- IBD-associated pyoderma gangrenosum is associated with clinically mild IBD, erythema nodosum, and female sex.
- Underlying bowel disease is active in over half of the patients at the time of an episode of pyoderma gangrenosum.
- Pyoderma gangrenosum is most often located on the lower extremity and can be periostomal.
- Ulcerative and pustular types of pyoderma gangrenosum may arise.
What causes pyoderma gangrenosum?
Pyoderma gangrenosum is an autoinflammatory disease (excessive response to an internal antigen) due to some form of neutrophil dysfunction. T lymphocytes and cytokines are involved. There may be a genetic predisposition.
Drugs are occasionally implicated as triggers of pyoderma gangrenosum, especially cocaine, isotretinoin, propylthiouracil, and sunitinib (a protein kinase inhibitor).
Injury to the skin is a common trigger (the pathergic response), and a surgical trigger is well known, and often misinterpreted as a wound infection.
What are the clinical features of pyoderma gangrenosum?
- Pyoderma gangrenosum usually starts quite suddenly, often at the site of a minor injury.
- It may start as a small pustule, red bump, or blood-blister, often misinterpreted as an insect bite.
- The skin then breaks down resulting in an ulcer. The ulcer can deepen and widen rapidly.
- Characteristically, the edge of the ulcer is purple and undermined.
- Pyoderma gangrenosum is usually very painful.
- Several ulcers may develop at the same time or over months to years.
Untreated, the ulcers may continue to enlarge, persist unchanged, or may slowly heal. Treatment is usually successful in arresting the process, but complete healing may take months. This is particularly true if there is an underlying venous disease, another reason for leg ulcers.
Deep ulcers heal with scarring, and this is sometimes with a characteristic cribriform (criss-cross pattern) or atrophic appearance. There are several rarer subtypes of pyoderma gangrenosum:
Bullous
- A superficial variant which can present with inflammatory bullae and superficial ulcers.
- Often be associated with haematological malignancy.
Pustular
- A variant normally seen in inflammatory bowel disease patients.
- Can present with pustules on an erythematous base.
Granulomatous superficial (vegetative)
- Can present with verrucous lesions and superficial ulceration.
- Typically distributed over the face and neck; associated systemic disease is rare.

Early haemorrhagic pyoderma gangrenosum

Ulceration, pustulation and the violaceos edge of pyoderma gangrenosum on the shin associated with ulcerative colitis

Bullous pyoderma gangrenosum with underlying ulcerative colitis

The erythematous and violaceous border typical of pyoderma gangrenosum above the knee

Multiple ulcers on the shin - the superior edge of the proximal ulcer showing the characterisitc purple edge
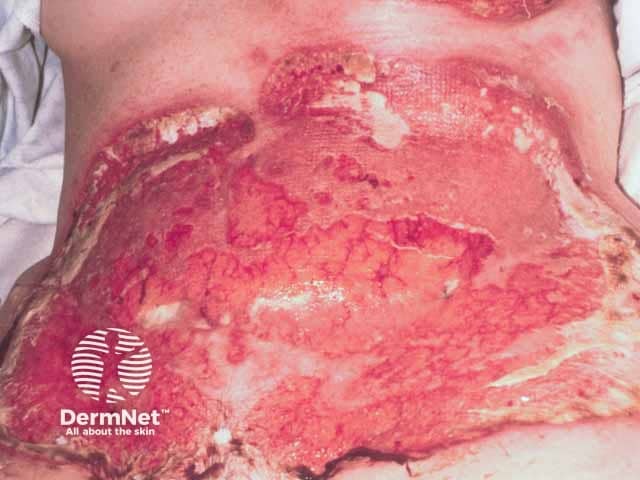
Severe pathergic pyoderma gangrenosum after breast cancer reconstructive surgery (TRAM procedure) (PG-patient1)

Healed post operative pyoderma gangrenosum after pulse intravenous methylprednisolone and ciclosporin (PG-patient1)

Multiple ulcers on the buttocks - note the violaceous oedematous ulcer edges
How is pyoderma gangrenosum diagnosed?
Pyoderma gangrenosum is diagnosed by its characteristic appearance and severe pain. The pathergy test is usually positive (a skin prick test causing a papule, pustule, or ulcer).
- The wound should be swabbed and cultured for microorganisms, but these are not the cause of pyoderma gangrenosum.
- A biopsy may be necessary to rule out other causes of ulceration. Pyoderma gangrenosum causes a neutrophilic inflammatory infiltrate, but this may be absent when on treatment.
- Mostly, blood tests are not particularly helpful. Some patients may have a positive ANCA (antineutrophil cytoplasmic antibody).
Maverakis criteria
Criteria published after a Delphi consensus exercise in 2018 supersede the Su criteria with a single major criterion required to diagnose pyoderma gangrenosum (a neutrophilic infiltrate). The addition of four or more of the eight minor criteria yields a sensitivity of 86% and a specificity of 90% for pyoderma gangrenosum.
Major criterion
- Histopathology of ulcer edge must show a neutrophilic infiltrate.
Minor criteria
- Exclusion of infection
- Pathergy
- History of inflammatory bowel disease or inflammatory arthritis
- History of papule, vesicle, or pustule ulcerating within four days
- Peripheral erythema, undermining border, and tenderness at the ulcer site
- Multiple ulcers, at least one on the anterior lower leg
- Cribriform or wrinkled paper scars at the site of the healed ulcer
- Decreased size of the ulcer within one month of initiating immunosuppressive medication.
What is the differential diagnosis of pyoderma gangrenosum?
Several other ulcerating conditions can mimic pyoderma gangrenosum such as:
- Venous or arterial ulcers
- Medium and large size vessel vasculitis
- Occlusive vasculopathy
- Ecthyma and ecthyma gangrenosum
- Ulcerating infections e.g. Buruli ulcer, tuberculosis
- Sporotrichosis
- Cutaneous amoebiasis
- Ulcerating skin tumours and lymphomas
- Drug induced ulcers e.g. iododerma, bromoderma, hydroxycarbamide, nicorandil
- Artefact.
What is the treatment of pyoderma gangrenosum?
Treatment of pyoderma gangrenosum is mainly non-surgical. The necrotic tissue should be gently removed. Wide surgical debridement should be avoided during the active stage of pyoderma gangrenosum because it may result in enlargement of the ulcer. Skin grafting and other surgical procedures may be performed when the active disease phase has settled, with care to minimise trauma.
Often conventional antibiotics such as flucloxacillin are prescribed before making the correct diagnosis. These may be continued if bacteria are cultured in the wound (secondary wound infection) or there is surrounding cellulitis (red hot, painful skin), but they are not helpful for uncomplicated pyoderma gangrenosum.
Small ulcers are often treated with:
- Potent topical steroid ointment
- Tacrolimus ointment
- Intralesional steroid injections into the ulcer edge
- Ciclosporin solution
- Special dressings
- Oral anti-inflammatory antibiotics such as doxycycline or minocycline
- If tolerated, careful compression bandaging to reduce swelling.
Systemic treatment for larger ulcers due to pyoderma gangrenosum may include:
- Oral prednisone for several weeks or longer, or intermittent intravenous methylprednisolone for 3–5 days
- Ciclosporin, which is as effective as prednisone and has differing adverse effects and risks
- Biologic agents: There is a growing body of evidence for success with the anti-TNF agents infliximab, adalimumab, etanercept; there are case reports of success with other biologic agents including ustekinumab, guselkumab, spesolimab, canakinumab, and anakinra.
- Small molecules, such as baricitinib.
Other therapies may include:
- Mycophenolate mofetil
- Dapsone
- Azathioprine
- A tetracycline such as minocycline
- Potassium iodide solution
- Methotrexate
- Cyclophosphamide
- Chlorambucil
- Intravenous immunoglobulins and plasmapheresis.
Expert wound care and pain management are essential. Once the disease is stable and inactive, surgical repair may be considered using a skin flap, skin graft, negative pressure wound therapy, and cultured skin.
Systemic therapy should be tapered slowly over several months.
What is the outlook for pyoderma gangrenosum?
The prognosis for pyoderma gangrenosum is unpredictable. About half of treated patients achieve wound healing on treatment with prednisone or ciclosporin within a year.
Patients with pyoderma gangrenosum should be very careful to avoid trauma, which can set off a new ulcer.
References
- Alavi A, French LE, Davis MD, Brassard A, Kirsner RS. Pyoderma Gangrenosum: An Update on Pathophysiology, Diagnosis and Treatment. Am J Clin Dermatol. 2017 Feb 21. doi: 10.1007/s40257-017-0251-7. [Epub ahead of print] Review. PubMed PMID: 28224502. PubMed
- Brenner M, Ruzicka T, Plewig G, Thomas P, Herzer P. Targeted treatment of pyoderma gangrenosum in PAPA (pyogenic arthritis, pyoderma gangrenosum and acne) syndrome with the recombinant human interleukin-1 receptor antagonist anakinra. Br J Dermatol. 2009;161(5):1199–201. Journal
- Charles CA, Leon A, Banta MR, Kirsner RS. Etanercept for the treatment of refractory pyoderma gangrenosum: a brief series. Int J Dermatol. 2007;46(10):1095–9. Journal
- George C, Deroide F, Rustin M. Pyoderma gangrenosum - a guide to diagnosis and management. Clin Med (Lond). 2019;19(3):224–8. Journal
- Keyal U, Liu Y, Bhatta AK. Dermatologic manifestations of inflammatory bowel disease: a review. Discovery Medicine 2018. Review
- Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti G. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol. 2009;23(9):1008–17. Journal
- Weenig RH, Davis MD, Dahl PR, Su WP. Skin ulcers misdiagnosed as pyoderma gangrenosum. N Engl J Med. 2002 Oct 31;347(18). PubMed
- Yamasaki K, Yamanaka K, Zhao Y, Iwano S, Takei K, Suzuki K, et al. Adalimumab in Japanese patients with active ulcers of pyoderma gangrenosum: Twenty-six-week phase 3 open-label study. J Dermatol. 2020;47(12):1383–90. Journal
On DermNet
- Pyoderma gangrenosum images
- Ulcers and erosions
- Neutrophilic dermatoses
- Sweet syndrome
- Neutrophilic dermatosis of hands
- Synthetic wound dressings
- Dermatological emergencies online course
- Skin manifestations of haematological disease
- Plasmapheresis for skin disease
- Skin signs of rheumatic disease
Other websites
- Dermatological emergencies — DermNet e-lecture [Youtube]
- Patient information: pyoderma gangrenosum (The Basics) — UpToDate (for subscribers)
- Pyoderma gangrenosum — British Association of Dermatologists
- Pyoderma gangrenosum — NORD rare diseases
