Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Pemphigus vulgaris pathology — extra information
Autoimmune/autoinflammatory Diagnosis and testing
Pemphigus vulgaris pathology
Author: Harriet Cheng BHB, MBChB, Dermatology Unit, Waikato Hospital; Duncan Lamont, Pathologist, Waikato Hospital; A/Prof Patrick Emanuel, Dermatopathologist, Auckland, New Zealand, 2013.
Pemphigus vulgaris is a chronic vesiculobullous skin disorder characterised by autoantibodies against desmoglein 3, which is a component of the desmosome (an intracellular adhesion molecule). Disruption of keratinocyte adhesion leads to superficial blistering and erosion affecting the skin and/or mucous membranes.
Histology of pemphigus vulgaris
Early lesions of pemphigus vulgaris show suprabasal epidermal acantholysis, clefting and blister formation. The blister cavity may contain inflammatory cells including eosinophils and rounded acantholytic cells with intensely eosinophilic cytoplasm and a perinuclear halo. The floor of the blister may be lined with intact keratinocytes, the “tombstone pattern” (figures 1, 2). Acantholysis can also affect adnexae. Dermal changes include perivascular inflammatory infiltrate particularly with eosinophils.
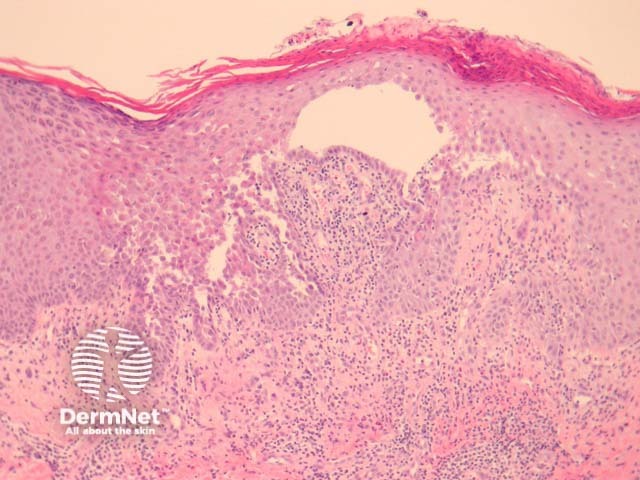
Figure 1
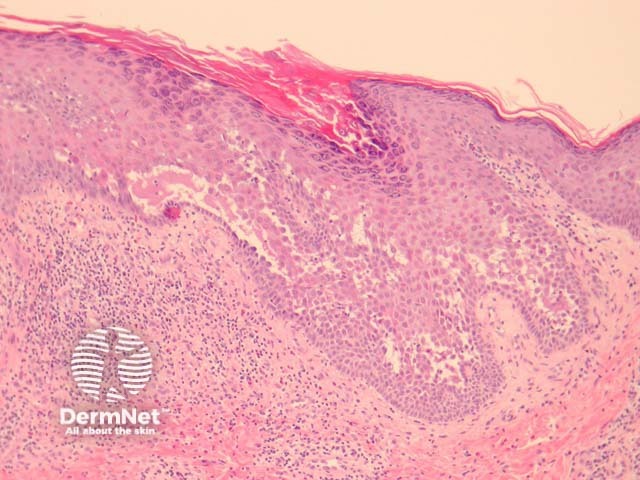
Figure 2
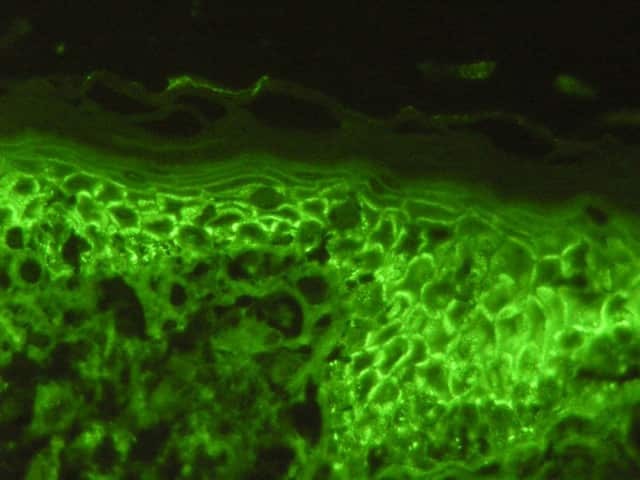
Figure 3
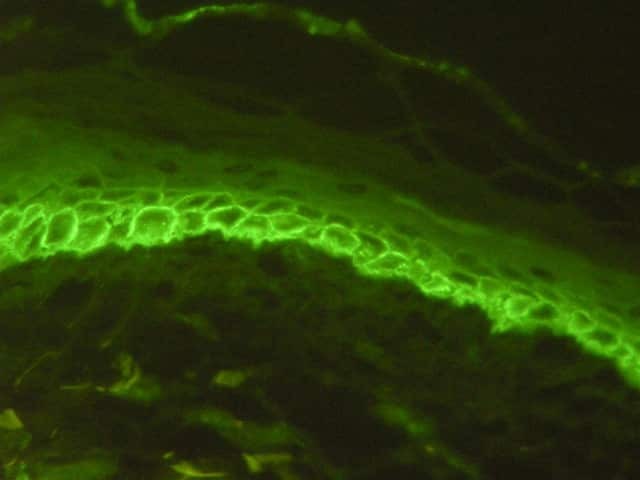
Figure 4
Special studies of pemphigus vulgaris
Direct immunofluorescence may be positive in perilesional skin with intercellular deposits of IgG and/or C3 in the epidermis (figures 3, 4). Antigen deposition can be seen in hair follicles (follicular outer root sheath and germinal matrix), meaning direct immunofluorescence may be positive when performed on plucked hair follicles.
Differential diagnosis of pemphigus vulgaris
Darier disease: Suprabasal clefting with dyskeratosis in the form of corps ronds and grains. Immunofluorescence is negative.
Hailey-Hailey disease: Disruption of epithelium adjacent to bullae (intact in pemphigus vulgaris) with sparing of adnexal structures. Immunofluorescence is negative.
Pemphigus foliaceus: Acantholysis more superficial within the granular layer. Lacks mucous membrane involvement.
Grover disease: There is a pemphigus-like form of this disease. Negative immunofluorescence and lack of adnexal involvement are helpful features.
References
- Dermatology (Third edition, 2012). Bolognia JL, Jorizzo JL, Schaffer JV
- Weedon’s Skin Pathology (Third edition, 2010). David Weedon
- Pathology of the Skin (Fourth edition, 2012). McKee PH, J. Calonje JE, Granter SR
On DermNet
