Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Pachyonychia congenita — extra information
Pachyonychia congenita
Author: Dr Sharnika Abeyakirthi, Dermatology Registrar, Waikato Hospital, Hamilton, New Zealand, 2014. Updated by Dr Fen-Lan Cherry Chang, House Officer, Middlemore Hospital, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. June 2020.
Introduction Demographics and causes Clinical features Classification Diagnosis Differential diagnoses Treatment Outcome
What is pachyonychia congenita?
Pachyonychia congenita is the name given to a group of rare, inherited disorders of keratinisation — the process by which keratin is formed and deposited in the outermost layer of the skin.
Pachyonychia congenita is characterised by thickened skin of the palms and soles, thickened nails, and white patches in mucous membranes. The specific features depend on which keratin gene is affected.

Plantar keratoderma

Pachyonychia congenita

Pachyonychia congenita
Who gets it and what is the cause of pachyonychia congenita?
The number of patients worldwide who have pachyonychia congenita is estimated to be somewhere between 1,000 and 10,000 [1]. The International Pachyonychia Congenita Research Registry (IPCRR) reported 977 individuals with genetically confirmed pachyonychia congenita in January 2020 [1].
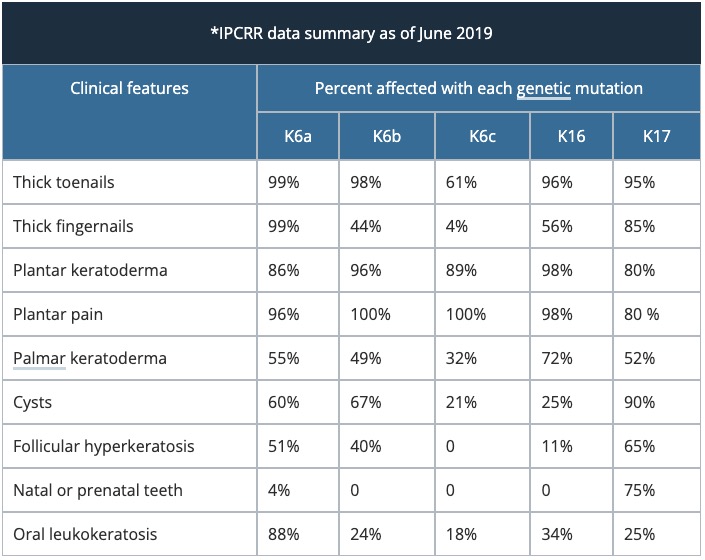
Pachyonychia congenita is caused by a mutation in the genes encoding keratin, K6a, K16, K17, K6b and K6c (listed in decreasing frequency). So far, 115 mutations have been described by the IPCRR.
Pachyonychia congenita is autosomal dominantly inherited. That means the defective gene comes from one parent. An affected person with an autosomal dominant disorder has a 50% chance of passing on the disease to his or her offspring at each pregnancy. It is found in all ethnic groups and in equal numbers in both sexes.
Pachyonychia congenita is often due to sporadic mutations during conception when patients do not report a family history.
What are the clinical features of pachyonychia congenita?
The clinical features of pachyonychia congenita depend on which keratin gene is involved.
Palms and soles
- Thickened or calloused palms and soles (palmoplantar hyperkeratosis or keratoderma, particularly focal palmoplantar keratoderma) cause difficulty in walking.
- Plantar plain affects 95% of patients with pachyonychia congenita; it may have a neuropathic component [3].
- The pain may be constant and severe particularly in patients with mutations of K6a and K16.
- Focal palmoplantar keratoderma may be the only feature of pachyonychia congenital in patients with mutations of K6c.
- Hyperhidrosis (excessive sweating) can accompany keratoderma.
- Blisters may be precipitated by friction and warm weather.

Pachyonychia congenita

Pachyonychia congenita
Nails
- Nail changes are most severe with mutations of K6a and K16.
- Nail thickening is apparent early in life — thus the name pachyonychia congenita.
- The nails often have a brownish discolouration.
- All fingernails are commonly involved; toenails to a lesser degree.
- Certain specific K16 mutations do not affect the fingernails.

Pachyonychia

Pachyonychia congenita

Pachyonychia congenita
Cysts
- Steatocystoma and pilosebaceous cysts are common.
- Almost all patients with mutations of K17 have steatocystoma multiplex.
- Cysts may or may not be painful.
Dry skin
- Friction sites such as knees and elbows may be dry due to follicular hyperkeratosis.
- Follicular hyperkeratosis tends to become less obvious in adult life.

Dry elbow skin
Mouth
- White patches affect the tongue and inside cheeks (leukokeratosis).
- Natal or prenatal teeth are uncommon and are typically a feature of K17 mutations.
- First bite syndrome — children with K6a mutation may experience intense pain when first beginning to eat.
- Children may develop angular cheilitis.

Oral leukokeratosis
Larynx
- Laryngeal involvement can vary from hoarseness of voice to airway obstruction [4].
Classification of pachyonychia congenita
Pachyonychia congenita was traditionally classified into Type 1 and Type 2, according to the clinical features. Classification now depends on which keratin gene has the specific mutation [2].
How is pachyonychia congenita diagnosed?
Pachyonychia congenita is usually diagnosed by its clinical appearance.
Skin biopsy of the affected tissues will only show nonspecific changes.
Molecular genetic studies can be done by specialist laboratories to detect mutations in the affected keratin genes. A genetic counsellor can advise whether the test is available in your area. Testing is available free of cost via Pachyonychia Congenita Project.
Prenatal testing is sometimes offered to pregnant women when they or a partner is affected by pachyonychia congenita. Pre-implantation diagnosis of ‘test-tube’ embryos has also been reported.
What is the differential diagnosis for pachyonychia congenita?
Prior to genetic testing, some patients were diagnosed with pachyonychia congenita that actually did not have this disorder. Mutations in other keratin genes can lead to similar skin conditions.
- Other genetic syndromes with similar features include Clouston syndrome, Olmsted syndrome, and palmoplantar keratoderma striata
- Steatocystoma multiplex
- Oral candidiasis
- Other nail disorders such as nail psoriasis or onychomycosis
What is the treatment for pachyonychia congenita?
There is, as yet, no cure for pachyonychia congenita. The effectiveness of a treatment depends on the severity of the specific problem.
Treatment of keratoderma might include:
- Mechanical debridement — regular trimming of the calluses can lessen pain
- Podiatry; nails should be trimmed to the appropriate length to reduce the risk of infections. Soaking beforehand can soften the skin/nails for easier trimming or clipping
- Emollient ointments
- Keratolytics, such as salicylic acid ointment, urea cream or other forms of heel balm
- Bleach baths to reduce infection
- Cushioned footwear and orthotics
- Pain relief.
Oral retinoids such as acitretin thin the calluses but have been shown to increase pain
Experimental treatments are being offered to some patients with pachyonychia congenita as part of clinical trials of novel agents such as mTOR inhibitors (eg, sirolimus).
What is the outcome for pachyonychia congenita?
Pachyonychia congenita does not affect lifespan but it has a significant impact on the individual’s quality of life due to the functional limitation and psychological effects produced by the disorder.
References
- Kaspar RL. Challenges in developing therapies for rare diseases including pachyonychia congenita. J Investig Dermatol Symp Proc 2005; 10: 62–6. DOI: 10.1111/j.1087-0024.2005.10208.x. PubMed
- Pachyonychia congenital project (accessed 7 June 2020)
- Brill S, Sprecher E, Smith FJD, Geva N, et al. Chronic pain in pachyonychia congenita: evidence for neuropathic origin. Br J Dermatol 2018; 179: 154–62. DOI: 10.1111/bjd.16217. PubMed
- O'Kane AM, Jackson CP, Mahadevan M, Barber C. Laryngeal manifestations of pachyonychia congenita: a clinical case and discussion on management for the otolaryngologist. J Laryngol Otol 2017; 131: S53–6. DOI: 10.1017/S0022215116008264. PubMed
On DermNet
- Scaly skin conditions
- Palmoplantar keratoderma
- Steatocystoma multiplex
- Nail disease
- Foot skin problems
- Hand skin problems
Other websites
- Pachyonychia Congenita Project
- Pachyonychia Congenita — Medscape Reference
- Pachyonychia congenita — US National Library of Medicine Genetics Home Reference
- Keratinization Disorders — geneSkin
- OMIM – Online Mendelian Inheritance in Man (search term pachyonychia congenita)
- Pachyonychia Congenita — GeneTests GeneReviews
