Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Intralesional injection — extra information
Intralesional injection
Author: Dr Tim Aung, Primary Care Practitioner, Brisbane & Logan, Queensland, Australia. DermNet Editor-in-Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. January 2020.
Introduction Uses Contraindications Medications Benefits Side effects and risks
What is an intralesional injection?
An intralesional injection is the direct injection of a therapeutic substance into a lesion or into the skin. The aim of an intralesional injection is to deliver a high concentration of medicine into the site of the pathology to maximise efficacy while minimising systemic adverse effects of the drug.
What drugs are used for intralesional injection and why?
The most common medication used for intralesional injection is a corticosteroid such as triamcinolone acetonide.
Intralesional steroid is used for localised inflammatory, hyperplastic, and hypertrophic lesions [1,2].
- Keloid and hypertrophic scar
- Immunological disorders such as:
- Lichenified skin disorders such as:
- Lichen simplex chronicus
- Nodular prurigo
- Hypertrophic lichen planus.
- Granulomatous skin disorders such as:
- Follicular disorders such as hidradenitis suppurativa and cystic acne
- Vascular disorders such as infantile haemangioma and pyogenic granuloma.
Other drugs that are sometimes injected into skin lesions include 5-fluorouracil (eg, for keloid scar) [3], bleomycin (eg, for viral wart) [4], methotrexate (eg, for nail psoriasis) [5], rose Bengal, and interferon (see Topical and intralesional immunotherapy for melanoma metastases).
Cosmetic use of injected substances include:
- Dermal fillers and augmentation procedures using collagen, hyaluronic acid, medical-grade silicone, autologous fat, and other agents
- Deoxycholic acid to reduce submental fat
- Botulinum toxin to reduce wrinkles.
What are the contraindications of intralesional injection?
The intralesional injection should not be used in or around an active bacterial skin infection (impetigo, atypical mycobacteria), fungal infection, or viral infection (herpes simplex).
It should not be used if the patient is allergic to the specific drug or excipient [6].
Intralesional injections may not be suitable for widespread or extensive lesions.
Medications, dosage and method of intralesional injection
Triamcinolone acetonide is widely available with 10 mg/mL or 40 mg/mL strengths marketed in Australasia. The dose depends on the type, size, and location of the lesion.
- 40 mg/mL is used for a large thick keloid scar.
- 5–10 mg/mL is used for a moderate thickness hypertrophic scar and other skin disorders.
- 2.5–5 mg/mL is used for a small lesion or a facial lesion [6].
0.1–0.2 mL is injected per square centimetre of involved skin. The steroid can be diluted with normal saline or plain local anaesthesic.
The medicine is placed in the dermis if it is a flat lesion (eg, alopecia areata), or within the lesion, if it is raised (eg, hypertrophic scar).
A Luer-lock syringe (figure 1) or an insulin syringe can be used with a 25 to 30-gauge needle, or a special syringe set with a controlled depth needle can be used (eg, Dermojet). Otherwise, the medicine may spill if the needle disconnects from the syringe due to the resistance of dense collagen tissue. Insert the needle at a 10 to 20-degree angle for a flat lesion (figure 2), or at an increased angle for a raised lesion. Subcutaneous injection should be avoided.
The procedure can be repeated every 4–6 weeks for 2–3 cycles or longer.

Figure 1: Luer-lock syringes
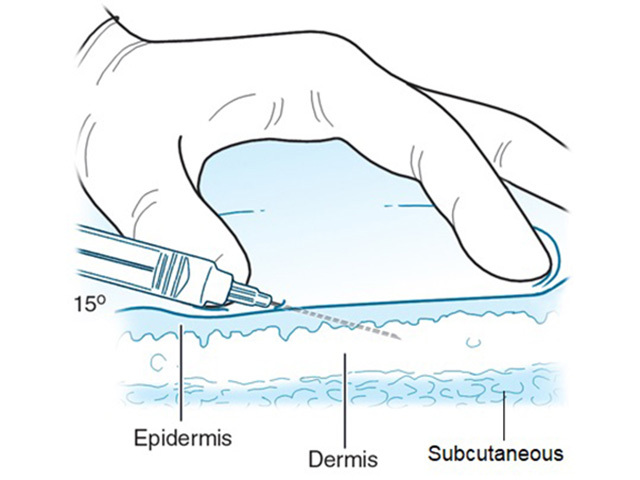
Figure 2: injecting into the superficial dermis

Figure 2 Credit: McGraw Hill Education; used with permission.
How to minimise the pain of intralesional injection
An intralesional injection is a painful procedure even when mixed with local anaesthetic, as numbing occurs a few minutes later. Tips for minimising pain are:
- Pre-treatment with topical lignocaine-prilocaine (EMLA) under occlusion one hour before the procedure (EMLA can penetrate to about 5 mm in healthy unbroken skin) [7]
- Pretreatment with an injection of local anaesthetic (lignocaine 1%) below the lesion; this has the advantage of elevating a scar, which makes it easier to infiltrate the steroid
- Pretreatment with cryotherapy to numb and soften the scar [2]
- A combination of local anaesthetic and cryotherapy; this may give increased efficacy and a better outcome [8–10].
What are the benefits of an intralesional injection?
An intralesional injection is a simple office-based and relatively safe procedure with proven benefits in specific skin conditions.
What are the side effects and risks of an intralesional injection?
The possible side effects of intralesional injection of a corticosteroid are:
- Short-term local pain, inflammatory reaction, and rarely, infection
- Longer-term hypopigmentation, hyperpigmentation, atrophy (more likely in the case of subcutaneous injection) and telangiectasia.
Approved datasheets are the official source of information for medicines, including approved uses, doses, and safety information. Check the individual datasheet in your country for information about medicines.
We suggest you refer to your national drug approval agency such as the Australian Therapeutic Goods Administration (TGA), US Food and Drug Administration (FDA), UK Medicines and Healthcare products regulatory agency (MHRA) / emc, and NZ Medsafe, or a national or state-approved formulary eg, the New Zealand Formulary (NZF) and New Zealand Formulary for Children (NZFC) and the British National Formulary (BNF) and British National Formulary for Children (BNFC).
References
- Mathes BM, Alguire PC. Intralesional injection. UpToDate. Updated 16 May 2017. Available at: www.uptodate.com/contents/intralesional-injection [accessed 10 April, 2018].
- Ustaine RP, Pfenninger JL, Stulberg DL, Small R. Intralesional injections. In: Dermatological and cosmetic procedures in office practice. Philadelphia: Saunders Elsevier; 2012. p. 199–208, 409.
- Prince GT, Cameron MC, Fathi R, Alkousakis T. Intralesional and laser-assisted 5-fluorouracil in dermatologic disease: A systematic review. J Drugs Dermatol. 2018 Mar 1;17(3):274-280. PMID: 29537445.PubMed
- Saitta P, Krishnamurthy K, Brown LH. Bleomycin in dermatology: a review of intralesional applications. Dermatol Surg. 2008 Oct;34(10):1299-313. doi:10.1111/j.1524-4725.2008.34281.x. Epub 2008 Jun 27. Review. PubMed
- Duarte AA, Carneiro GP, Murari CM, Jesus LCB.Nail psoriasis treated with intralesional methotrexate infiltration. An Bras Dermatol. 2019 Oct 17;94(4):491-492. doi: 10.1590/abd1806-4841.20198170. eCollection 2019. PubMed
- Premanshu B, Prateek M, Swarn L. Intralesional steroid injections: look before you leap! Indian J Dermatol. 2014 Jul;59(4):410-1. doi: 10.4103/0019-5154.135506. PMID: 25071269; PMCID: PMC4103286. PubMed Central
- Azad S, Sacks L. Painless steroid injections for hypertrophic scars and keloids. Br J Plast Surg. 2002 Sep;55(6):534. doi: 10.1054/bjps.2002.3913. PMID: 12479437. PubMed
- Yosipovitch G, Widijanti Sugeng M, Goon A, Chan YH, Goh CL. A comparison of the combined effect of cryotherapy and corticosteroid injections versus corticosteroids and cryotherapy alone on keloids: a controlled study. J Dermatolog Treat. 2001 Jun;12(2):87-90. doi: 10.1080/095466301317085363. PMID: 12243664. PubMed
- Juckett G, Hartman-Adams H. Management of keloids and hypertrophic scars. Am Fam Physician. 2009 Aug 1;80(3):253-60. PMID: 19621835. PubMed
- Boutli-Kasapidou F, Tsakiri A, Anagnostou E, Mourellou O. Hypertrophic and keloidal scars: an approach to polytherapy. Int J Dermatol. 2005 Apr;44(4):324-7. doi: 10.1111/j.1365-4632.2004.02570.x. PMID: 15811088. PubMed
On DermNet
- Intralesional steroid injection
- Topical and intralesional immunotherapy for melanoma metastases
- Keloid and hypertrophic scar
- Injected skin treatments
Other websites
- Intralesional injections — Medline Plus
