Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Colloid milium — extra information
Colloid milium
Authors: Dr Frank Po-Chao Chiu, Senior House Officer, Royal Brisbane and Women’s Hospital, Brisbane, QLD, Australia; Dr Jim Muir, Dermatologist, South East Dermatology, Brisbane, QLD, Australia. Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. July 2019.
Introduction
Classification
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
What is colloid milium?
Colloid milium refers to a group of rare, degenerative, cutaneous deposition disorders.
The colloid degeneration disorders are characterised by amorphous, hyaline-like deposits in the dermis, which classically present as yellow–brown, semi-translucent papules and plaques over sun-exposed areas [1].

Adult colloid milium

Adult colloid milium

Adult colloid milium
How is colloid milium classified?
There are currently five different subtypes of colloid milium:
- Adult colloid milium
- Juvenile colloid milium
- Pigmented colloid milium
- Nodular colloid degeneration (paracolloid) of the skin
- Acral keratosis with eosinophilic dermal deposits [2].
Since colloid milium was first described as “Das Colloid-Milium der Haut” by Dr Ernst Wagner in 1866, it has also been known as colloid degeneration, colloid pseudomilium, miliary colloidoma, colloid infiltration hyaloma, and elastosis colloidalis conglomerata [3].
Who gets colloid milium?
Adult colloid milium is the most commonly occurring subtype and typically develops in fair-skinned men aged 30–60 years with an outdoor occupation, such as farming [1]. Men are four times more likely than women to develop adult colloid milium. Medical conditions occasionally associated with adult colloid milium include multiple myeloma and beta-thalassaemia [1,2].
Juvenile colloid milium is exceedingly rare. It tends to develop between 10 and 20 years of age, but it has occurred in a child aged 4 years [4]. Familial cases of juvenile colloid milium with an autosomal recessive inheritance have been reported [5].
Pigmented colloid milium usually follows the use of hydroquinone bleaching creams and extensive sun exposure. A case of pigmented colloid milium that was not associated with hydroquinone has also been reported in a Caucasian farmer with chronic exposure to fertilisers and sunlight [6].
There have been 13 reported cases of nodular colloid degeneration since it was first described in 1927; eight cases occurred in males, and the mean age was 52 years (range: 25–76 years) [7,8].
A series of six elderly Caucasians were reported to have acral keratosis with eosinophilic dermal deposits; four were male, with a mean age of 74 years (range: 59–81 years).
What are the causes of colloid milium?
Adult colloid milium is associated with exposure to excessive sunlight, petroleum, and chemicals, although its pathogenesis remains unclear. It is suspected that sunlight ruptures elastin fibres resulting in an accumulation of proteins or fibroblast products in the dermis. Contributing factors may include trauma and photodynamic effects of phenols in gas oil [3].
Juvenile colloid milium is associated with chronic sun exposure and severe sunburn, resulting in keratinocyte degeneration [4].
Pigmented colloid milium is associated with ochronosis due to hydroquinone in bleaching creams and sun exposure [1].
The role of sun exposure in nodular colloid degeneration is uncertain as a case has been described involving the penis [7]. The colloid material is suspected to relate to actinic degeneration of elastic fibres (solar elastosis) [7].
The cause of acral keratosis with eosinophilic dermal deposits is unknown. It may involve sun exposure and the regression of viral warts, although evidence for active human papillomavirus infection has not been observed [9,10].
What are the clinical features of colloid milium?
Adult colloid milium typically presents with numerous flesh-coloured or yellow–brown, semi-translucent, dome-shaped papules, that are 1–4 mm in diameter.
- Papules can coalesce into plaques.
- They tend to occur in sun-exposed areas of the face, ears, neck, dorsum of hands, and forearms.
- Unilateral involvement on the sun-exposed arm has been reported in taxi and truck drivers [2].
- A soft, golden-coloured gelatinous material can often be expressed with pressure [11].
- The underlying skin may be hypertrophic and hyperpigmented [12].
- Lesions are asymptomatic or transiently itchy [1].
Dermoscopy reveals yellow–brown clods.
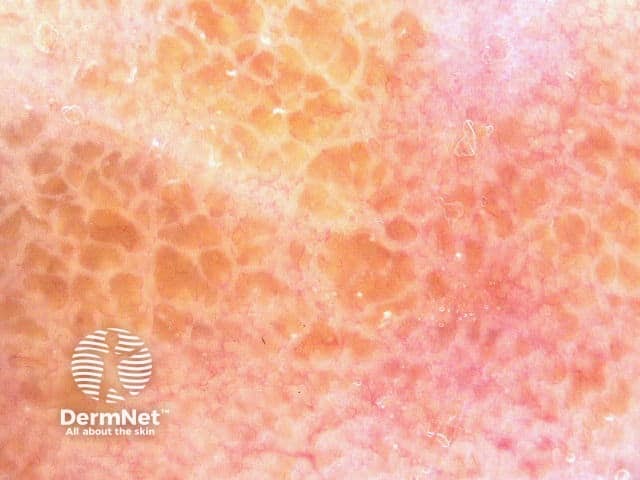
Dermoscopy of adult colloid milium
Pigmented colloid milium is characterised by grey–black clustered papules on the face [6].
Nodular colloid degeneration presents as an isolated nodule or plaque, approximately 50 mm in diameter, on chronically sun-exposed skin, particularly the face. The scalp, trunk, and extremities can also be affected [12].
Acral keratosis with eosinophilic dermal deposits presents as painless, slowly-progressive, hyperkeratotic papules on the palmar or dorsal aspects of the fingers [2,10].
What are the complications of colloid milium?
There are no systemic complications of adult colloid milium.
Juvenile colloid milium has been reported to induce ligneous conjunctivitis, a rare disease characterised by wood-like pseudomembranes developing on the mucous membrane of the eye (ocular and extraocular mucosae), and periodontitis, although the pathogenesis of these is unclear [1,14].
How is colloid milium diagnosed?
Colloid milium is confirmed by skin biopsy [12]; (see the DermNet page on colloid milium pathology). Colloid milium can be distinguished from amyloidosis and other conditions by using special stains, immunohistochemistry, and electron microscopy [1].
Histopathology of colloid milium
Histopathological features of adult colloid milium include:
- Deposits of homogenous, amorphous, faintly eosinophilic material with dividing clefts and fissures, which extend into the papillary and mid-dermis [2,3]
- Fibroblasts lining the clefts, which can contain lymphocytes and mast cells [12]
- Lack of inflammation
- Preserved adnexae (skin appendages, including sebaceous glands, sweat glands, and hair follicles) [15]
- Dilated blood vessels surrounding the colloid deposits [1,12]
- Solar elastosis with a Grenz zone separating the colloid deposits from the overlying epidermis [2,12,16]
- A flattened or hyperkeratotic epidermis [3]
In contrast to adult colloid milium, juvenile colloid milium lacks a Grenz zone and the colloid substance is found within the epidermis or superficial dermis [13].
In acral keratosis with eosinophilic dermal deposits, deposits of amorphous eosinophilic material are localised to the papillary dermis. This colloid milium subtype is not associated with elastotic degeneration (the breakdown of elastic tissue) or fissuring.
Electron microscopy
Under electron microscopy, the colloid ultrastructure appears as medium electron-dense, amorphous, granular material with short, ill-defined, branching filaments that are much smaller than those seen in amyloidosis [1,2]. Desmosome remnants, active fibroblasts, binding proteins, and nuclear proteins have also been observed [2,12].
Special stains
Adult colloid milium stains positive with crystal violet, Congo red, and periodic acid–Schiff (PAS) stains [2,11]. Adult colloid milium also stains a 'robin's egg blue' with the Pinkus' acid orcein–Giemsa stain and will fluoresce with thioflavin T [2].
Immunohistochemistry is often necessary to distinguish colloid milium from amyloidosis. Both adult colloid milium and amyloidosis stain positive for amyloid P protein. Unlike amyloidosis, adult colloid milium displays negative reactivity to cytokeratin (including MNF-116), laminin, type IV collagen, cotton dyes (including pagoda red), and light chain immunoglobulin (Ig) [11,17]. Adult colloid milium stains positively for IgG, IgM, and NKH-1 antigen (a stain for proteins related to elastic fibre microfibrils) [4].
Juvenile colloid milium does not stain for amyloid P protein but does stain positive with antikeratin and cytokeratin antibodies (including MNF116 and cytokeratin AE1/AE3) [2,13]. Juvenile colloid milium also stains positive for IgG within the colloid deposits [18]. Positive pan-cytokeratin labelling and use of electron microscopy suggest that juvenile colloid milium deposits derive from degenerate, epidermal keratinocytes in contrast to adult colloid milium, where deposits are suspected to derive from degenerate elastic tissue in the dermis [5].
Colloid islands of both the pigmented colloid milium and nodular colloid degeneration subtypes are found in the upper dermis, with fissures and clefts that extend deep within the dermis [2,6,19]. Additional yellow–brown, banana–shaped ochronotic fibres are also seen between the collagen and elastin bundles of the deep dermis in the pigmented colloid milium subtype [6].
The pigmented colloid milium and nodular colloid degeneration subtypes both stain positive with PAS and elastin stains but are negative for Congo red, in contrast to the adult colloid milium subtype [6,7].
In acral keratosis with eosinophilic dermal deposits, the deposits are positive with trichrome and PAS staining, while staining negative for Congo red, amyloid P protein, type IV collagen, and cytokeratin antibodies [2].
What is the differential diagnosis for colloid milium?
The differential diagnosis of colloid milium includes other conditions presenting with multiple papules [1,11,12]. This may include:
- Milium/milia
- Sebaceous hyperplasia
- Syringomas
- Retention cysts
- Molluscum contagiosum
- Systemic and primary cutaneous amyloidosis
- Steatocystoma multiplex
- Lipoid proteinosis
- Calcinosis cutis
- Cutaneous sarcoidosis
- Papular mucinosis.
What is the treatment for colloid milium?
Treatment may include combinations of medical and physical therapies [1,11,12].
Medical therapies
Medical therapies to treat colloid milium include:
- Topical retinoids (tretinoin, isotretinoin, and adapalene)
- Keratolytic creams (urea, salicylic acid, and alpha hydroxy acids).
Physical therapies
Physical therapies to treat colloid milium include:
- Curettage and electrosurgery
- Cryotherapy
- Dermabrasion
- Carbon dioxide or erbium laser resurfacing
- Photodynamic therapy.
Excessive cautery, cryotherapy, and laser therapy may cause poor cosmetic results [3].
What is the outcome for colloid milium?
Colloid milium may become more extensive over time, but it tends to stabilise after 3 years [3]. New lesions rarely develop after this period. If left untreated, colloid milium typically persists with no spontaneous resolution [1].
References
- Rongioletti F. Colloid milium. In: Smoller BR, Rongioletti F (eds). Clinical and pathological aspects of skin diseases in endocrine, metabolic, nutritional and deposition disease. New York: Springer New York, 2010: 157–160.
- Patterson JW. Weedon's skin pathology, 4th edn. Edinburgh: Churchill Livingstone/Elsevier, 2016: 423–56.
- Siadat A, Mokhtari F. Colloid milium. Adv Biomed Res 2013; 2: 28. DOI: 10.4103/2277-9175.107996. PubMed Central
- Hashimoto K, Nakayama H, Chimenti S, et al. Juvenile colloid milium: Immunohistochemical and ultrastructural studies. J Cutan Pathol 1989; 16: 164–74. DOI: 10.1111/j.1600-0560.1989.tb00033.x. PubMed
- Handfield‐Jones SE, Atherton DJ, Black MM, Hashimoto K, McKee PH. Juvenile colloid milium: clinical, histological and ultrastructural features. J Cutan Pathol 1992; 19: 434–8. DOI: 10.1111/j.1600-0560.1992.tb00617.x. PubMed
- Akhyani M, Hatami P, Yadegarfar Z, Ghanadan A. Pigmented colloid milium associated with exogenous ochronosis in a farmer with long-term exposure to fertilizers. J Dermatol Case Rep 2015; 9: 42–5. DOI: 10.3315/jdcr.2015.1197. PubMed Central
- Choi JW, Kim CB, Park JE, Cho JH, Kim HK, Kim JK. Nodular colloid degeneration. Am J Dermatopathol 2011; 33: 388–91. DOI: 10.1097/DAD.0b013e3181e3d294. PubMed
- Chu H, Kim HJ, Lee MG. Xanthoma‐like multiple yellowish nodular colloid degeneration on the face and scalp. J Eur Acad Dermatol Venereol 2017; 31: e195–6. DOI: 10.1111/jdv.13937. PubMed
- Rübben A, Kalka K, Spelten B, Grußendorf-Conen E-I. Clinical features and age distribution of patients with HPV 2/27/57-induced common warts. Arch Dermatol Res 1997; 289: 337–40. DOI: 10.1007/s004030050201. PubMed
- Saeed S, Sagatys E, Morgan MB. Acral keratosis with eosinophilic dermal deposits: a distinctive clinicopathologic entity or colloid milium redux? J Cutan Pathol 2006; 33: 679–85. DOI: 10.1111/j.1600-0560.2006.00530.x. PubMed
- Zeinab AS, Omid Z, Rudolph RI. Nodular colloid milium mimicking keloid. J Cosmet Dermatol 2017; 16: e45–7. DOI: 10.1111/jocd.12325. PubMed
- Zamora AB, Simón MP, Sánchez AT, Ponce Olivera RM. Adult colloid milium. An underdiagnosed and difficult to treat entity. Rev Med Hosp Gen (Mex) 2016; 79: 21–5. DOI: 10.1016/j.hgmx.2015.10.002. Journal
- Muscardin LM, Bellocci M, Balus L. Papuloverrucous colloid milium: an occupational variant. Br J Dermatol 2000; 143: 884–7. DOI: 10.1046/j.1365-2133.2000.03798.x. PubMed
- Azad N, Zafar S, Khan A. Successful treatment of ligneous conjunctivitis with topical cyclosporine and heparin. J AAPOS 2009; 13: 519–20. DOI: 10.1016/j.jaapos.2009.06.005. PubMed
- Alsaad KO, Obaidat NA, Ghazarian D. Skin adnexal neoplasms — part 1: An approach to tumours of the pilosebaceous unit. J Clin Pathol 2007; 60: 129–44. DOI: 10.1136/jcp.2006.040337. PubMed Central
- Abbas O, Mahalingam M. The grenz zone. Am J Dermatopathol 2013; 35: 83–91. DOI: 10.1097/DAD.0b013e31824feb4e. PubMed
- Prieto VG, Lugo J, McNutt NS. Intermediate‐ and low‐molecular‐weight keratin detection with the monoclonal antibody MNF116. An immunohistochemical study on 232 paraffin‐embedded cutaneous lesions. J Cutan Pathol 1996; 23: 234–41. DOI: 10.1111/j.1600-0560.1996.tb01472.x. PubMed
- Ebner H, Gebhart W. Colloid milium: light and electron microscopic investigations. Clin Exp Dermatol 1977; 2: 217–26. DOI; 10.1111/j.1365-2230.1977.tb02561.x. PubMed
- Ghanadan A, Kamyab-Hesari K, Daneshpajouh M, Balighi K, Normohammadpour P. Nodular colloid degeneration of the skin: Report of three cases with review and update. Indian Dermatol Online J 2014; 5(Suppl 1): S36–9. DOI: 10.4103/2229-5178.144527. PubMed Central
On DermNet
Other websites
- Colloid milium — Medscape
