Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Xanthoma — extra information
Xanthoma
Authors: Vanessa Ngan, Staff Writer; Dr Amy Stanway, Dermatology Registrar, Nottingham, United Kingdom, 2005. Updated by Dr Helen Gordon, Medical Editor, Auckland, New Zealand. Copy edited by Gus Mitchell. October 2020.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
What is a xanthoma?
A xanthoma is a skin lesion caused by the accumulation of fat in macrophages in the skin. Less commonly, a xanthoma will occur in a subcutaneous layer.
Who gets xanthomas?
Xanthomas are usually a skin sign of disorders of lipid metabolism (dyslipidaemias) or occur in histiocytosis; the former is the focus of this page. Xanthomas typically affect adults, although children with familial hypercholesterolaemia may present with xanthomas. The race and sex distributions depend on the underlying cause.
What causes xanthomas?
Dyslipidaemias causing xanthomas are classified as primary or secondary.
Primary dyslipidaemias
Primary dyslipidaemias associated with xanthomas can include:
- Hypercholesterolaemia eg, familial type
- Combined dyslipidaemia, eg, Type III hyperlipoproteinaemia
- Hypertriglyceridaemia, eg, Types I, IV, and V hyperlipoproteinaemia
- Cerebrotendinous xanthomatosis and sitosterolaemia.
Secondary dyslipidaemias
Secondary dyslipidaemias associated with xanthomas include:
- Obesity
- Diabetes mellitus and insulin resistance
- Cholestatic liver disease, such as primary biliary cirrhosis
- Nephrotic syndrome
- Medications, such as:
- Oestrogens
- Tamoxifen
- Oral retinoids
- Prednis(ol)one
- Ciclosporin.
Diffuse plane xanthomatosis is associated with paraproteinaemia. Xanthoma disseminatum is a rare form of histiocytosis.
What are the clinical features of xanthoma?
There are multiple types of xanthomas, and they are classified by their clinical presentation.
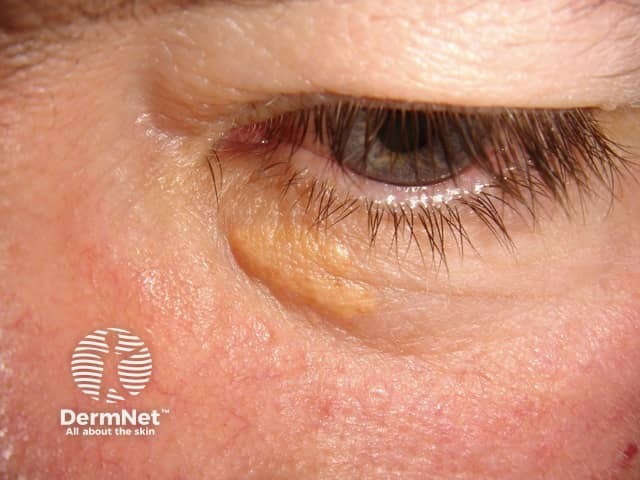
Xanthelasma
Xanthelasma (also known as xanthelasma palpebrarum or xanthelasma palpebrum), is the most common form of xanthoma. It is a type of plane xanthoma usually located around the medial canthus of the upper eyelid. Upper and lower eyelids can be affected symmetrically.
Xanthelasma:
- Starts as a small bump that enlarges slowly over several months.
- Presents as soft, yellow or yellow-orange macules, papules, or plaques.
- Is associated with familial hypercholesterolaemia, Type II hyperlipoproteinaemia, and primary biliary cirrhosis.
- Will often occur with normal levels of circulating lipids.


See more images of xanthelasma.
Other plane xanthomas
Plane xanthomas (planar xanthoma, plane xanthomatosis) are soft, yellow macules or patches that can occur anywhere on the body. Involvement of the webspace between the fingers and toes is pathognomonic for homozygous familial hypercholesterolaemia. Plane xanthomas may also be associated with Type III hyperlipoproteinaemia, and need to be distinguished from diffuse plane xanthomatosis.
Palmar xanthoma
Palmar xanthoma (xanthoma striata palmaris) present as a yellow-orange accentuation of the palmar and wrist creases. This is diagnostic for Type III hyperlipoproteinaemia.
Tuberous xanthoma
Tuberous xanthomas are firm, painless, red-yellow nodules that develop over pressure areas such as the knees, elbows, and heels. They may join together to form large multilobulated masses. Tuberous xanthomas are often associated with Type III hyperlipoproteinaemia.


Tendon xanthoma
Tendon xanthomas (tendinous xanthoma) are slowly enlarging subcutaneous nodules usually found attached to the Achilles tendon or tendons over the knuckles. They are smooth, firm to palpation, and mobile. The overlying skin colour is normal. Tendon xanthomas are most commonly associated with familial hypercholesterolaemia, but can also be seen in cerebrotendinous xanthomatosis and sitosterolaemia.

Eruptive xanthoma
Eruptive xanthomas typically present as crops of 2–5 mm yellow papules with a red rim over extensor surfaces such as the buttocks or shoulders, but can be widespread including inside the mouth. The papules may be tender and are usually itchy. They may demonstrate köbnerisation. Eruptive xanthomas are due to hypertriglyceridaemia (triglyceride >11.2 mmol/L) of any cause.



Verruciform xanthoma
Verruciform xanthoma is a rare entity not associated with dyslipidaemias. It most commonly affects the mouth, where it is found as a solitary, asymptomatic lesion on the gingiva and is associated with chronic graft-versus-host disease. On the genitalia, it has been called a Vegas (verruciform genital-associated) xanthoma and presents as a yellow-brown or red verrucous plaque. The lipid found in the foamy macrophages is thought to derive from keratinocytes, and it is possibly a reaction to chronic irritation.
What are the complications of xanthoma?
Xanthoma is usually a sign skin of a dyslipidaemia and therefore the complications are those of the underlying condition, such as pancreatitis or cardiovascular disease. Xanthelasma appears to be an independent predictor of ischaemic heart disease, separate from any associated dyslipidaemia.
How is xanthoma diagnosed?
Xanthoma is often a clinical diagnosis made in the setting of a dyslipidaemia. Skin biopsy may be required and shows the characteristic lipid-filled macrophages in the dermis (see Eruptive xanthoma pathology).
Investigations are required to determine the associated condition and may include:
- Lipid profile
- Liver, thyroid, and renal function tests
- Fasting blood glucose
- Serum and urine protein electrophoresis for diffuse plane xanthomas.
What is the differential diagnosis for xanthoma?
Xanthomas may need to be distinguished from many other skin lesions depending on the clinical presentation.
- Tuberous and tendon xanthomas — consider rheumatoid nodules, gouty tophi
- Eruptive xanthomas — need to be distinguished from xanthoma disseminatum
- Verruciform xanthoma — can resemble a genital wart
- Plane xanthomas — must be distinguished from eruptive plane xanthomatosis.
What is the treatment for xanthoma?
Some xanthomas resolve with successful treatment of the underlying dyslipidaemia: tuberous, eruptive, plane, and palmar. Xanthelasma may improve if associated with hypercholesterolaemia and this can be successfully treated. However treatment of the lesions may be required for cosmetic reasons and can include topical trichloroacetic acid (see Chemical peels), electrodessication, cryotherapy, laser vaporisation (see Nd:YAG, Er:YAG, carbon dioxide laser), or excision. Verrucous xanthoma is surgically excised and rarely recurs.
Trichloroacetic acid treatment of xanthelasma

Before trichloroacetic acid treatment

During trichloroacetic acid treatment

One month after treatment
Laser treatment of xanthelasma

Xanthelasma: after laser ablation
What is the outcome for xanthoma?
The importance of diagnosing xanthomas is recognising the associated trigger and its complications. The prognosis therefore depends on the successful management of the underlying medical condition.
References
- Flynn PD. Xanthomas and abnormalities of lipid metabolism and storage. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D (eds). Rook’s Textbook of Dermatology [4 volumes], 9th edn. Wiley Blackwell, 2016: 62.2-6.
- Nair PA, Singhal R. Xanthelasma palpebrarum - a brief review. Clin Cosmet Investig Dermatol. 2017;11:1–5.doi:10.2147/CCID.S130116. PubMed Central
- Rallidis LS, Iordanidis D, Iliodromitis E. The value of physical signs in identifying patients with familial hypercholesterolemia in the era of genetic testing [published online ahead of print, 2020 Jul 30]. J Cardiol. 2020;S0914-5087(20)30237-9. doi:10.1016/j.jjcc.2020.07.005. Journal
- Rothschild M, Duhon G, Riaz R, et al. Pathognomonic palmar crease xanthomas of apolipoprotein E2 homozygosity-familial dysbetalipoproteinemia. JAMA Dermatol. 2016;152(11):1275–6. doi:10.1001/jamadermatol.2016.2223. PubMed
- Santos MA, Foulke G. Koebnerization and eruptive xanthomas. J Gen Intern Med. 2019;34(9):1947–8. doi:10.1007/s11606-019-05178-1. PubMed
- Stiff KM, Cohen PR. Vegas (verruciform genital-associated) xanthoma: A comprehensive literature review. Dermatol Ther (Heidelb). 2017;7(1):65–79. doi:10.1007/s13555-016-0155-0. PubMed Central
- Tamiolakis P, Theofilou VI, Tosios KI, Sklavounou-Andrikopoulou A. Oral verruciform xanthoma: report of 13 new cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2018;23(4):e429–35. doi:10.4317/medoral.22342. PubMed Central
- Zak A, Zeman M, Slaby A, Vecka M. Xanthomas: clinical and pathophysiological relations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(2):181–8. doi:10.5507/bp.2014.016. PubMed
On DermNet
Other websites
- Xanthomas — Medscape Reference
- Search term 'Xanthoma' — Online Mendelian Inheritance in Man
