Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Sézary syndrome — extra information
Lesions (cancerous) Systemic diseases
Sézary syndrome
Authors: Dr Samir Seleq, PGY2 House Officer, Auckland Public Hospital, New Zealand; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand; June 2015.
DermNet Update May 2021. Copy edited by Gus Mitchell.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is Sézary syndrome?
Sézary syndrome is a rare leukaemic variant of cutaneous T-cell lymphoma (CTCL) defined by the triad of erythroderma, lymphadenopathy, and atypical malignant Sézary cells in the skin, blood, and lymph nodes.

Sézary syndrome

Sézary syndrome
Who gets Sézary syndrome?
Sézary syndrome typically presents in patients 55–60 years of age, with a male predominance (2:1). The annual incidence is estimated to be 1/10,000, with a higher incidence in black skin over white. Sézary syndrome comprises 3% of all cases of CTCL.
What causes Sézary syndrome?
Sézary syndrome arises from a skin tropic memory CD41 T-cell. The role of Staphylococcus aureus superantigen or chronic antigen stimulation has been proposed to lead to clonal expansion of T-cell and malignant transformation.
Sézary cells show diverse and complex chromosomal anomalies affecting many cellular pathways. Many genetic alterations have been identified in recent large-scale surveys, providing information on the molecular pathogenesis and offering new therapeutic targets under investigation.
A viral aetiology has not been identified.
Rare cases of malignancy including Sézary syndrome during treatment with JAK inhibitors have been reported. Causality has not been established and requires further investigation.
What are the clinical features of Sézary syndrome?
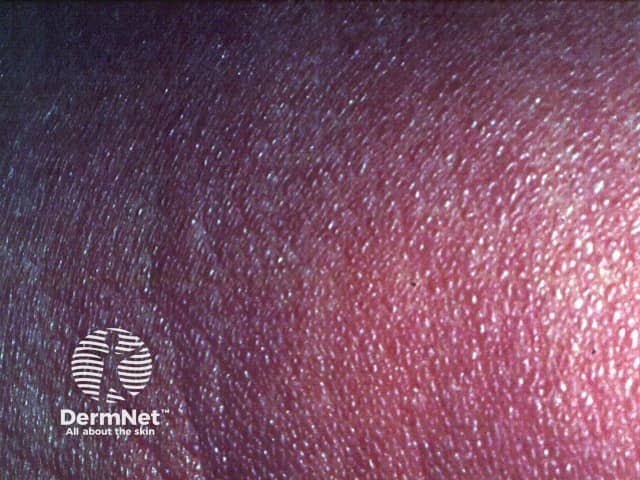
- Erythroderma (>80% body surface area) — diffuse erythema, often appears eczematous, variable scale
- Itch
- Rapid onset
- Rarely preceded by mycosis fungoides
- Sometimes prodrome of pruritus +/- non-specific dermatitis
- Other non-essential cutaneous manifestations — palmoplantar keratoderma, alopecia, ectropion, nail dystrophy — commonly paronychia, leukonychia, onycholysis are seen but onychoschizia, onychauxis, distal notching and anonychia seem to be more specific changes [see Nail terminology]
- Other frequent but non-essential clinical features — lymphadenopathy, hepatosplenomegaly

Erythroderma

Nail change

Plantar keratoderma
How do clinical features vary in differing types of skin?
Sézary syndrome presents at a younger age in black patients than white (53 v 63 years of age) and survival is worse regardless of age and stage at diagnosis.
Dermoscopy of Sézary syndrome
- White scale and dotted vessels — 100%
- Linear vessels and brown dots — 66%
- Patchy perifollicular brown dots — most characteristic
What are the complications of Sézary syndrome?
- Impact on quality of life — itch, difficulty falling asleep, anxiety, depression
- Increased risk of bacterial infection due to disruption of the skin barrier and immunosuppression which correlates with the malignant T-cell burden
- Complications of erythroderma due to any cause
- Large-cell transformation of the original malignant clone — defined as a skin biopsy with more than 25% of the dermal infiltrate being composed of cells >4 times the size of a small lymphocyte — poor prognostic sign
How is Sézary syndrome diagnosed?
Sézary syndrome should be considered in the differential diagnosis for any patient presenting with erythroderma.
International Society for Cutaneous Lymphomas (ISCLE) criteria for diagnosis
- Clinical — erythroderma, generalised lymphadenopathy
- Histopathologic — Skin biopsy histology may not be diagnostic and may be difficult to distinguish from mycosis fungoides [see Mycosis fungoides pathology]. Overlying acanthosis, dermal fibrosis, striking cerebriform nuclear atypia, minimal epidermotropism, and a sparse superficial perivascular infiltrate may be clues. Immunohistochemistry: CD4+ cells
- Lymph node histology — complete effacement of nodal architecture by infiltrating Sézary cells
- Immunophenotyping — flow cytometry of peripheral blood shows at least 1000 Sézary cells per mm3, CD4:CD8 ratio >10, CD4+/CD7- >30%, CD4+/CD26- >40%, aberrant expression of pan-T-cell antigens
- Molecular studies — high throughput sequencing of the T-cell receptor (TCR) beta gene CDR3 region shows clonally related T-cells (Sézary cells) in the skin, peripheral blood, and lymph nodes.
Imaging may include: chest x-ray, lymph node field ultrasound, CT, MRI, PET.
Staging for MF/SS: TNMB (tumour, node, metastasis, blood) – Sézary syndrome must, by definition, be T4 – erythroderma, N0-3, B2 – Sezary cells >1000/mm3 in peripheral blood, M0-1.
What is the differential diagnosis for Sézary syndrome?
- Erythrodermic mycosis fungoides
- All other causes of erythroderma
What is the treatment for Sézary syndrome?
Effective symptom relief
- Gabapentin (anticonvulsant)
- Mirtazapine (antidepressant)
Long-term disease control
- Extracorporeal photopheresis — methoxsalen is approved by the PBS in Australia for this indication
- Total skin electron beam therapy
- Systemic therapies
- Monoclonal antibodies
- Alemtuzumab — targets CD52 to deplete circulating T-cells and B-cells
- Mogamulizumab — targets C-C chemokine receptor 4 (CCR4) – approved by PDMA (Japan, 2012), FDA (US, 2018), and TGA (Australia, 2021) for Sézary syndrome after at least one prior systemic therapy
- Allogeneic stem cell transplant — only potentially curative option
Control of life-threatening complications
- Fluid and protein replacement
- Temperature maintenance
- Systemic antibiotics for infection
What is the outcome for Sézary syndrome?
Poor prognostic factors for Sézary syndrome:
- Age over 60 years
- Advanced stage of disease — Stage IV
- >80% body surface area (BSA) involvement
- Elevated lactate dehydrogenase.
The median survival of Sézary syndrome is estimated to be 3–5 years with a five-year survival of less than 30%.
References
- Damasco FM, Geskin L, Akilov OE. Onychodystrophy in Sézary syndrome. J Am Acad Dermatol. 2018;79(5):972-3. doi:10.1016/j.jaad.2018.06.023 Journal
- Dobos G, Pohrt A, Ram-Wolff C, et al. Epidemiology of cutaneous T-cell lymphomas: a systematic review and meta-analysis of 16,953 patients. Cancers (Basel). 2020;12(10):2921. doi:10.3390/cancers12102921. Journal
- Hristov AC, Tejasvi T, Wilcox RA. Mycosis fungoides and Sézary syndrome: 2019 update on diagnosis, risk-stratification, and management. Am J Hematol. 2019;94(9):1027–41. doi:10.1002/ajh.25577. Journal
- Kandai Saito and others, A case of Sézary syndrome in a patient during treatment with baricitinib for seronegative rheumatoid arthritis, Clinical and Experimental Dermatology, Volume 48, Issue 4, April 2023. Journal
- Larocca C, Kupper T. Mycosis fungoides and Sézary syndrome: an update. Hematol Oncol Clin North Am. 2019;33(1):103–20. doi:10.1016/j.hoc.2018.09.001. PubMed Central
- Pulitzer M. Cutaneous T-cell lymphoma. Clin Lab Med. 2017;37(3):527–46. doi:10.1016/j.cll.2017.06.006. PubMed Central
- Scarisbrick JJ, Bagot M, Ortiz-Romero PL. The changing therapeutic landscape, burden of disease, and unmet needs in patients with cutaneous T-cell lymphoma. Br J Haematol. 2021;192(4):683–96. doi:10.1111/bjh.17117. Journal
- Sławińska M, Sokołowska-Wojdyło M, Olszewska B, Nowicki RJ, Sobjanek M, Zalaudek I. Dermoscopic and trichoscopic features of primary cutaneous lymphomas - systematic review. J Eur Acad Dermatol Venereol. 2021;10.1111/jdv.17219. doi:10.1111/jdv.17219. PubMed
- Sławińska M, Sokołowska-Wojdyło M, Sobjanek M, Golińska J, Nowicki RJ, Rudnicka L. The significance of dermoscopy and trichoscopy in differentiation of erythroderma due to various dermatological disorders. J Eur Acad Dermatol Venereol. 2021;35(1):230–40. doi:10.1111/jdv.16998. Journal
- Stadler R, Scarisbrick JJ. Maintenance therapy in patients with mycosis fungoides or Sézary syndrome: a neglected topic. Eur J Cancer. 2021;142:38–47. doi:10.1016/j.ejca.2020.10.007. PubMed
- Vonderheid EC, Bernengo MG, Burg G, et al. Update on erythrodermic cutaneous T-cell lymphoma: report of the International Society for Cutaneous Lymphomas. J Am Acad Dermatol. 2002;46(1):95–106. doi:10.1067/mjd.2002.118538. PubMed
- Willemze R, Cerroni L, Kempf W, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood. 2019;133(16):1703–14. doi:10.1182/blood-2018-11-881268. Journal
On DermNet
- Cutaneous T-cell lymphoma
- Erythroderma
- Mycosis fungoides
- Skin manifestations of haematological diseases
Other websites
- Sezary syndrome — Genetics Home Reference
- Sezary syndrome — Orphanet
- Sezary syndrome — Genetic and Rare Diseases Information Center (GARD)
