Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Epithelial sheath neuroma — extra information
Epithelial sheath neuroma
Authors: Dr Akshay Flora, Resident Medical Officer, Royal Prince Alfred Hospital, University of Sydney, Central Clinical School, Sydney, NSW, Australia; Dr Roger (Hyun Joon) Kim, Anatomical Pathology Registrar, Douglas Hanly Moir Pathology, Sydney, NSW, Australia. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. June 2020.
Introduction Demographics Causes Clinical features Diagnosis Differential diagnoses Treatment and outcome
Submit your photo for epithelial sheath neuroma
What is an epithelial sheath neuroma?
Epithelial sheath neuroma is a rare benign cutaneous tumour composed of dermal nerve fibres surrounded by squamous epithelium [1,2].
Who gets epithelial sheath neuroma?
Epithelial sheath neuroma has so far only been reported in 13 people; all have been older than 40 years of age. It has been reported most commonly in females [1].
What causes an epithelial sheath neuroma?
The pathogenesis of epithelial sheath neuroma has not been determined, however several possible mechanisms have been suggested.
- A reactive hyperplasia of peripheral nerves and epithelium in response to an external stimulus or to entrapment of epithelium within the perineurium (a sheath of connective tissue) [3].
- Squamous metaplasia of the perineurium of enlarged nerve bundles as a reaction to localised inflammation [4].
- Neural crest remnants from embryonal development that differentiated into neural and squamous epithelial elements [5].
- Interleukin 6-mediated hyperplasia in response to localised inflammation or minor trauma at the site of a previous skin biopsy [6].
What are the clinical features of epithelial sheath neuroma?
Epithelial sheath neuroma presents as a persistent erythematous papule or nodule located on the upper or mid-back. Some patients report tenderness, pruritus, or paraesthesia when the lesion is palpated [1].
How is epithelial sheath neuroma diagnosed?
Epithelial sheath neuroma is diagnosed by histopathological examination of a skin biopsy. It is characterised by multiple enlarged peripheral nerve fibres that are sheathed by mature squamous epithelium. Epithelial sheath neuroma is sometimes surrounded by myxoid (mucus-like) stroma and a lymphocytic infiltrate.
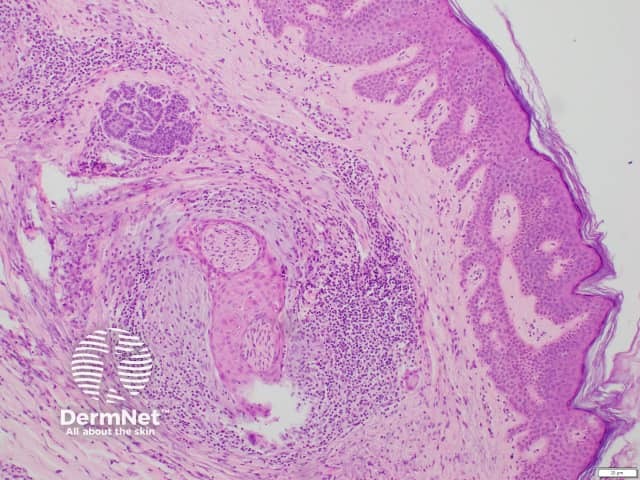
Histology of epithelial sheath neuroma
What is the differential diagnosis for epithelial sheath neuroma?
The clinical differential diagnosis for epithelial sheath neuroma may include:
- Squamous cell carcinoma
- Basal cell carcinoma
- Inflamed cyst
- Inflamed or irritated melanocytic naevus.
The histological differential diagnosis for epithelial sheath neuroma includes reactive neuroepithelial aggregates, perineural invasion of a well-differentiated cutaneous carcinoma, or re-excision perineural invasion [7,8].
What is the treatment and outcome of epithelial sheath neuroma?
Epithelial sheath neuroma is benign.
The treatment of choice is excision, with no reports of recurrence after excision to date [1].
References
- Flora A, Kim RH, Lara Rivero AD, Carr U, Isaacs F. Epithelial sheath neuroma: a case series. JAAD Case Rep. 2020;6(3):240-2. doi:10.1016/j.jdcr.2020.01.018. PubMed Central
- Requena L, Grosshans E, Kutzner H, et al. Epithelial sheath neuroma: a new entity. Am J Surg Pathol. 2000;24(2):190-6. doi:10.1097/00000478-200002000-00004. PubMed
- Zelger BG, Zelger B. Epithelial sheath neuroma: a benign neoplasm?. Am J Surg Pathol. 2001;25(5):696-8. doi:10.1097/00000478-200105000-00024. PubMed
- Kutzner H. For Valentine's Day: epithelial sheath neuroma. Cancer. 2001;91(4):804-5. doi: 10.1002/1097-0142(20010215)91:4<804::Aid-cncr1067>3.0.Co;2-t. PubMed
- Dunn M, Morgan MB, Beer TW, Chen KT, Acker SM. Histologic mimics of perineural invasion. J Cutan Pathol. 2009;36(9):937-42. doi:10.1111/j.1600-0560.2008.01197.x. PubMed
- Wang JY, Nuovo G, Kline M, Magro CM. Reexcision perineural invasion and epithelial sheath neuroma possibly on a spectrum of postinjury reactive hyperplasia mediated by IL-6. Am J Dermatopathol. 2017;39(1):49-52. doi:10.1097/DAD.0000000000000671. PubMed
- Chen KT. Reactive neuroepithelial aggregates of the skin. Int J Surg Pathol. 2003;11(3):205-10. doi:10.1177/106689690301100307. PubMed
- Stern JB, Haupt HM. Reexcision perineural invasion. Not a sign of malignancy. Am J Surg Pathol. 1990;14(2):183-5. doi:10.1097/00000478-199002000-00010. PubMed
On DermNet
