Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Angioimmunoblastic T-cell lymphoma — extra information
Angioimmunoblastic T-cell lymphoma
Authors: Dr Flora Poon, Victorian Dermatology Registrar, St. Vincent’s Hospital, Melbourne, VIC, Australia; Dr Christopher Y Chew, Medical Resident, Monash Health, Melbourne, VIC, Australia; Dr Rubeta N Matin, Consultant Dermatologist, Oxford University Hospitals, Oxford, UK. DermNet Editor in Chief: Adjunct A/Prof. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. March 2020.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is angioimmunoblastic T-cell lymphoma?
Angioimmunoblastic T-cell lymphoma is a rare nodal peripheral T-cell lymphoma (PTCL) that results in systemic symptoms and profound immune deficiency [1]. It sometimes causes a rash.
Angioimmunoblastic T-cell lymphoma is characterised histologically by a polymorphous infiltrate primarily involving lymph nodes, a proliferation of high endothelial venules, and follicular dendritic cells [2].
Who gets angioimmunoblastic T-cell lymphoma?
Angioimmunoblastic T-cell lymphoma is rare.
- Peripheral T-cell lymphomas comprise 10–15% of all lymphoid malignancies [1,3]
- Angioimmunoblastic T-cell lymphoma accounts for 15–20% of peripheral T-cell lymphomas and 1–2% of non-Hodgkin lymphomas [2,4].
Typically, angioimmunoblastic T-cell lymphoma affects older adults [4]. The median age of diagnosis is 62–65 years. Incidence is equal in men and women [4].
No risk factors have been identified for angioimmunoblastic T-cell lymphoma.
What causes angioimmunoblastic T-cell lymphoma?
The cell of origin of angioimmunoblastic T-cell lymphoma is the follicular helper T-cell [4]. Malignant transformation has been associated with mutations in the epigenetic regulators (TET2, IDH2 and DNMT3A), the Ras homolog gene family member A (RHOA) and T-cell receptor pathway (CD28, FYN, PLCG1, CARD11, P13K elements, CTNNB1, and GTF2I) [4].
Angioimmunoblastic T-cell lymphoma is promoted by the overexpression of angiogenic mediators (factors that regulate the development of blood vessels), such as vascular endothelial growth factor (VEGF) and interleukin (IL)-8, and cytokines that are proinflammatory (IL6, IL18), immunosuppressive (IL10), or induce proliferation (IL21) [4,5].
Infectious diseases associated with angioimmunoblastic T-cell lymphoma include Epstein-Barr virus (EBV, the cause of infectious mononucleosis), human herpesvirus 6 (HHV-6) (the cause of roseola), HHV-8 (the cause of Kaposi sarcoma), human immunodeficiency virus (HIV), bacterial infections and fungal infections [4].
The role of Epstein Barr virus
EBV establishes lifelong persistent infection in B cells. The immunodeficiency caused by angioimmunoblastic T-cell lymphoma reactivates EBV [4,6–8].
- EBV-infected B cells are present in 58–97% of patients with angioimmunoblastic T-cell lymphoma [8,9].
- EBV (and potentially HHV-6) may play a role in promoting disease progression through modulation of cytokines, chemokines, and membrane receptors [6].
- EBV is thought to prolong the life span of the B-cell and may cause genetic aberrations, such as preventing c-myc-induced apoptosis, leading to B-cell lymphoma [4,8,10]. See Epstein–Barr virus-associated lymphoproliferative disorders.
What are the clinical features of angioimmunoblastic T-cell lymphoma?
More than 70% of patients with angioimmunoblastic T-cell lymphoma present with constitutional symptoms. These include fevers, chills, night sweats, malaise, weight loss, arthralgias, and in 50%, a rash [11].
Lymphadenopathy and hepatosplenomegaly are typically present on examination. Pleural effusions, ascites, neurological signs, and gastrointestinal symptoms are less common [4].
Cutaneous features of angioimmunoblastic T-cell lymphoma
Angioimmunoblastic T-cell lymphoma most often presents with a non-specific rash [11]. It can also result in papules, nodules, plaques, ulcers, petechiae, and, rarely, erythroderma [8,11,12].
Rash associated with angioimmunoblastic T-cell lymphoma

Eroded papules and plaques in paraneoplastic pemphigus
What are the complications of angioimmunoblastic T-cell lymphoma?
Patients with angioimmunoblastic T-cell lymphoma are at increased risk of a secondary B-cell lymphoma, particularly diffuse large B-cell lymphoma (DLBCL), and less commonly, Hodgkin lymphoma, or plasmacytoma [13].
There are 30 documented cases of EBV-associated B-cell lymphomas in patients with angioimmunoblastic T-cell lymphoma (November 2019) [14–16].
EBV-induced diffuse large B-cell lymphoma can also present with cutaneous signs, including ulcerated papules, nodules, and abscesses [16].
How is angioimmunoblastic T-cell lymphoma diagnosed?
Laboratory abnormalities include:
- Anaemia (often haemolytic, with a positive Coombs test)
- Eosinophilia
- Polyclonal hypergammaglobulinaemia
- Antinuclear antibodies (ANA)
- Cold agglutinins
- Cryoglobulinaemia
- Circulating immune complexes
- Elevated serum lactate dehydrogenase (LDH) and beta-2-microglobulin
- Elevated EBV.
Peripheral blood leukocytosis with lymphocytosis is uncommon. Flow cytometry can be used to detect aberrant T-cells [17].
The diagnosis of angioimmunoblastic T-cell lymphoma is typically established by lymph node biopsy.
There are five angioimmunoblastic T-cell lymphoma histopathological patterns in the skin.
- A superficial perivascular infiltrate composed of eosinophils and lymphocytes that lack atypia (the most common pattern)
- A sparse perivascular infiltrate with atypical lymphocytes
- A dense superficial and deep infiltrate of pleomorphic lymphocytes
- Vasculitis, with or without atypical lymphocytes
- Necrotising granulomas.
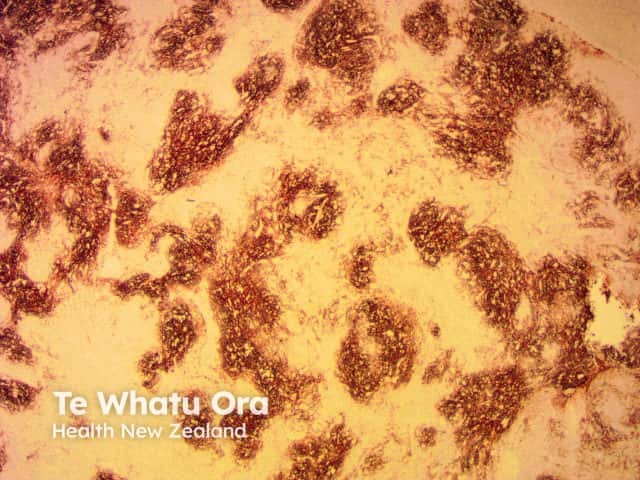
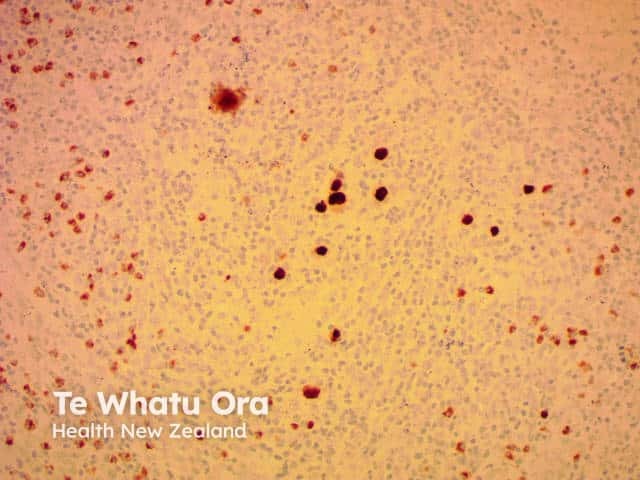
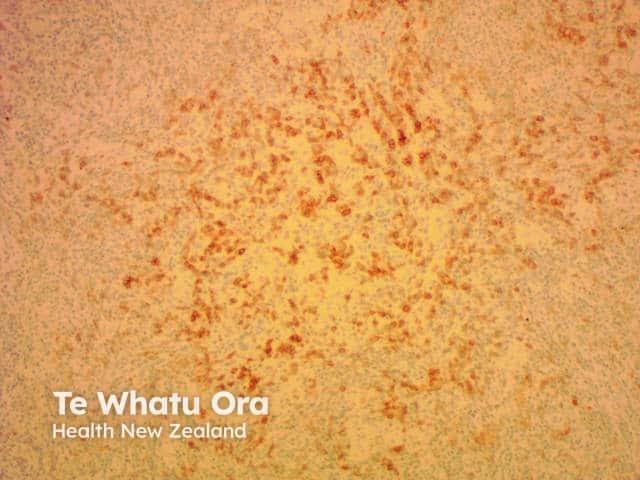
Histology of angioimmunoblastic T-cell lymphoma


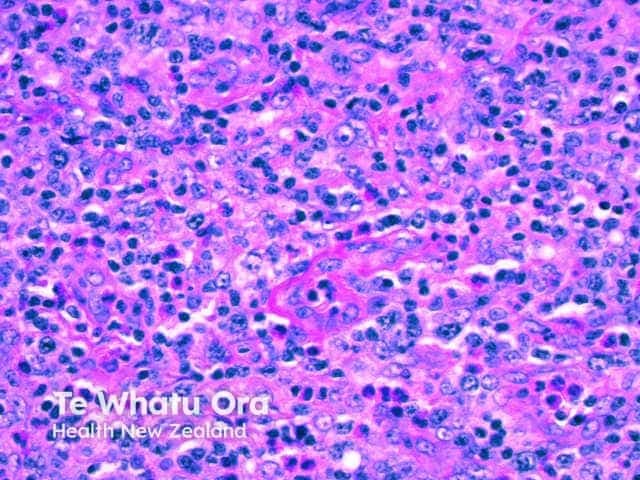
The immunophenotype of neoplastic cells typically corresponds to follicular T-helper cells (CD3+, CD4+, CD8−, CD10+, PD-1+, ICOS+, Bcl-6+, chemokine ligand CXCL13+) plus clusters of CD21+ follicular dendritic cells.
EBV positivity found on an immunohistochemistry stain is reportedly higher in more mature lesions and occasionally forms diffuse patterns [18].
Immunohistochemistry of angioimmunoblastic T-cell lymphoma


What is the differential diagnosis for cutaneous angioimmunoblastic T-cell lymphoma?
The differential diagnosis of cutaneous angioimmunoblastic T-cell lymphoma depends on the morphology of the cutaneous rash, but can include:
- Drug eruption
- Viral exanthem
- Atypical mycobacterial infection or another opportunistic infection
- Other causes of erythroderma.
What is the treatment for angioimmunoblastic T-cell lymphoma?
Due to the rarity of angioimmunoblastic T-cell lymphoma, therapy is generally guided by prospective phase II studies [4].
- The most common treatment is anthracycline-based chemotherapy such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone/prednisolone).
- Follow-up consolidation with autologous stem-cell transplantation has shown promising results [19].
- Trials of histone deacetylase (HDAC) inhibitors, hypomethylating agents, and anti-CD30 antibodies are on-going [20–23].
What is the outcome for angioimmunoblastic T-cell lymphoma?
Angioimmunoblastic T-cell lymphoma is typically aggressive with a median survival of fewer than 3 years, even with intensive treatment. Patients usually present with late stage III-IV disease, and survival rates have been quoted as being 33% 5 years and 29% at 7 years [18].
- Standard CHOP chemotherapy has an overall response rate of 70–80% and 5-year progression-free survival of 10–20% [8,24].
- Follow-up BEAM (carmustine, etoposide, cytarabine, melphalan) and autologous stem-cell transplantation have a 5-year progression-free survival rate of around 40% [25].
Circulating EBV DNA levels may be monitored; higher levels are associated with poorer prognosis. However, the presence of EBV in nodal tumours does not alter prognosis.
Secondary B-cell lymphomas have a typically poor prognosis. Eight out of 30 patients with EBV-associated B-cell lymphoma survived beyond 12 months [14–16].
References
- Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375-90. doi:10.1182/blood-2016-01-643569. PubMed
- Carbone A, Gloghini A, Dotti G. EBV-associated lymphoproliferative disorders: classification and treatment. Oncologist. 2008;13(5):577-585. doi:10.1634/theoncologist.2008-0036. PubMed
- Jaffe ES, Ralfkiaer E. Mature T-cell and NK-cell neoplasms. In: Jaffe ES, Harris NL, Stein H, et al (eds). World Health Organisation Classification of Tumours, Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissue. Lyon, France: IARC Press, 2001: 189–235.
- Yabe M, Dogan A, Horwitz S, Moskowitz A. Angioimmunoblastic T-cell lymphoma. Cancer Treat Res. 2019;176:99-126. doi:10.1007/978-3-319-99716-2_5. PubMed
- Iqbal J, Wright G, Wang C, et al. Gene expression signatures delineate biological and prognostic subgroups in peripheral T-cell lymphoma. Blood. 2014;123(19):2915-23. doi:10.1182/blood-2013-11-536359. PubMed Central
- Bräuninger A, Spieker T, Willenbrock K, et al. Survival and clonal expansion of mutating "forbidden" (immunoglobulin receptor-deficient) epstein-barr virus-infected b cells in angioimmunoblastic t cell lymphoma. J Exp Med. 2001;194(7):927-40. doi:10.1084/jem.194.7.927. PubMed
- Zhou Y, Attygalle A, Chuang S, et al. Angioimmunoblastic T-cell lymphoma: histological progression associates with EBV and HHV6B viral load. Br J Haematol. 2007;138(1):44-53. doi:10.1111/j.1365-2141.2007.06620.x. PubMed
- Dogan A, Gaulard P, Jaffe ES, et al. Angioimmunoblastic T-cell lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al (eds). WHO Classification of Tumours of Haematotopoetic and Lymphoid Tissues, 4th edn, Lyon, France: IARC Press; 2008: 309–11.
- Attygalle A, Chuang S, Diss T, Du M, Isaacson P, Dogan A. Distinguishing angioimmunoblastic T-cell lymphoma from peripheral T-cell lymphoma, unspecified, using morphology, immunophenotype and molecular genetics. Histopathology. 2007;50(4):498-508. doi:10.1111/j.1365-2559.2007.02632.x. PubMed
- Allday M. How does Epstein-Barr virus (EBV) complement the activation of Myc in the pathogenesis of Burkitt's lymphoma?. Semin Cancer Biol. 2009;19(6):366-376. doi:10.1016/j.semcancer.2009.07.007. PubMed
- De Leval L, Gisselbrecht C, Galard P. Advances in the understanding and management of angioimmunoblastic T-cell lymphoma. Br J Haematol. 2010;148(5):673-89. doi:10.1111/j.1365-2141.2009.08003.x. PubMed
- Martel P, Laroche L, Courville P, et al. Cutaneous involvement in patients with angioimmunoblastic lymphadenopathy with dysproteinemia: a clinical, immunohistological, and molecular analysis. Arch Dermatol. 2000;136(7):881-886. doi:10.1001/archderm.136.7.881. PubMed
- Willenbrock K, Bräuninger A, Hansmann M. Frequent occurrence of B-cell lymphomas in angioimmunoblastic T-cell lymphoma and proliferation of Epstein-Barr virus-infected cells in early cases. Br J Haematol. 2007;138(6):733-9. doi:10.1111/j.1365-2141.2007.06725.x. PubMed
- Şimşek C, Bostankolu B, Özoğul E, Sağlam Ayhan A, Üner A, Büyükaşık Y. EBV-Related Diffuse Large B-Cell Lymphoma in a Patient with Angioimmunoblastic T-Cell Lymphoma. Turk J Haematol. 2019;36(1):57-59. doi:10.4274/tjh.galenos.2018.2018.0023. PubMed Central
- Szablewski V, Dereure O, René C, et al. Cutaneous localization of angioimmunoblastic T-cell lymphoma may masquerade as B-cell lymphoma or classical Hodgkin lymphoma: A histologic diagnostic pitfall. J Cutan Pathol. 2019;46(2):102-10. doi:10.1111/cup.13382. PubMed
- Poon F, Ieremia E, Collins G, Matin RN. Epstein-Barr Virus-induced cutaneous diffuse large B-cell lymphoma in a patient with angioimmunoblastic T-cell llymphoma. Am J Dermatopathol. 2019;41(12):927-30. doi:10.1097/DAD.0000000000001371. PubMed
- Singh A, Schabath R, Ratei R, et al. Peripheral blood sCD3⁻ CD4⁺ T cells: a useful diagnostic tool in angioimmunoblastic T cell lymphoma. Hematol Oncol. 2014;32(1):16-21. doi:10.1002/hon.2080. PubMed
- Massoni C, Winfield HL, Smoller BR. Other lymphoproliferative and myeloproliferative dseases. In: Bolognia J, Schaffer J, Cerroni L. Dermatology [2 volumes]. 4th edn. London: Elsevier, 2018: 2148-59.
- d'Amore F, Relander T, Lauritzsen G, Jantunen E, Hagberg H, Anderson H et al. Up-Front Autologous Stem-Cell Transplantation in Peripheral T-Cell Lymphoma: NLG-T-01. J Clin Oncol 2012; 30: 3093–99. DOI: 10.1200/JCO.2011.40.2719. PubMed
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Feb 29, 2000. Identifier NCT01796002, Efficacy and Safety of Romidepsin CHOP vs CHOP in Patients With Untreated Peripheral T-Cell Lymphoma; 2013 February 13 [cited Oct 06, 2019]. Available from: https://clinicaltrials.gov/ct2/show/study/NCT01796002
- Horwitz S, O'Connor O, Pro B, et al. Brentuximab vedotin with chemotherapy for CD30-positive peripheral T-cell lymphoma (ECHELON-2): a global, double-blind, randomised, phase 3 trial. Lancet 2019; 393: 229–40. DOI: 10.1016/S0140-6736(18)32984-2. PubMed
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Feb 29, 2000. Identifier NCT03161223, Durvalumab in Different Combinations With Pralatrexate, Romidepsin and Oral 5-Azacitidine for Lymphoma; 2017 May 19 [cited Oct 06, 2019]. Available from: https://clinicaltrials.gov/ct2/show/NCT03161223
- O'Connor O, Falchi L, Lue J, et al. Oral 5-azacytidine and romidepsin exhibit marked activity in patients with PTCL: A multicenter phase I study. Blood 2019; 134: 1395–1405. DOI: 10.1182/blood.2019001285. PubMed
- Savage K, Chhanabhai M, Gascoyne R, Connors J. Characterisation of peripheral T-cell lymphomas in a single North American institution by the WHO classification. Ann Oncol 2004; 15: 1467–75. DOI: 10.1093/annonc/mdh392. PubMed
- Mehta N, Maragulia J, Moskowitz A, et al. A retrospective analysis of peripheral T-cell lymphoma treated with the intention to transplant in the first remission. Clin Lymphoma Myeloma Leuk 2013; 13: 664–70. DOI: 10.1016/j.clml.2013.07.005. PubMed
On DermNet
- Lymphoma
- Cutaneous T-cell lymphoma
- Cutaneous B-cell lymphoma
- Hodgkin lymphoma
- Intravascular lymphoma
- Epstein–Barr virus-associated lymphoproliferative disorders
Other websites
- Angioimmunoblastic lymphoma — Cancer Research UK
- Angioimmunoblastic T-Cell Lymphoma — NORD
- Angioimmunoblastic T-Cell Lymphoma — Lymphoma Research Foundation
- Angioimmunoblastic T-Cell Lymphoma — Macmillan Cancer Support
- Angioimmunoblastic T-cell lymphoma (AITL) and follicular T-cell lymphoma (FTCL) — Lymphoma Action
- Angioimmunoblastic T cell lymphoma: What every physician needs to know — Cancer Therapy Advisor
- Angioblastic T cell lymphoma — PathologyOutlines.com
