Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Wound dressings
Created in 2009.
Learning objectives
- Describe dressings used for:
- Necrotic wounds
- Sloughy wounds
- Granulating wounds
- Epithelialising wounds
- Infected wounds
- Describe bioengineered skin substitutes in outline
Introduction
Good wound care will minimize the inflammatory response, speed healing and minimize scarring.
Dressings for acute wounds
Sterile dressings should be applied to acute wounds, including those due to skin surgery, for the following reasons.
- Keep the wound clean and prevent contamination by foreign bodies.
- Apply pressure to encourage haemostasis and prevent haematoma
- Immobilise the wound
- Reduce the risk of bacterial infection.
- Absorb drainage of blood or wound exudate
- Occlusion provides thermal insulation.
- Allow for oxygen entry and water vapour escape
- To cover the wound for cosmetic reasons.
These goals can be accomplished with a layered dressing comprised of a bottom, nonadherent contact layer, a middle layer that can absorb wound exudate and exert pressure, and an outer covering of tape or a rolled bandage. Sterile dressings come in various sizes from simple gauze pads to adhesive bandages.
Melolin non-adherent dressing Assorted Nexcare plasters for acute wounds Melolin non-adherent dressing Assorted Nexcare plasters for acute wounds 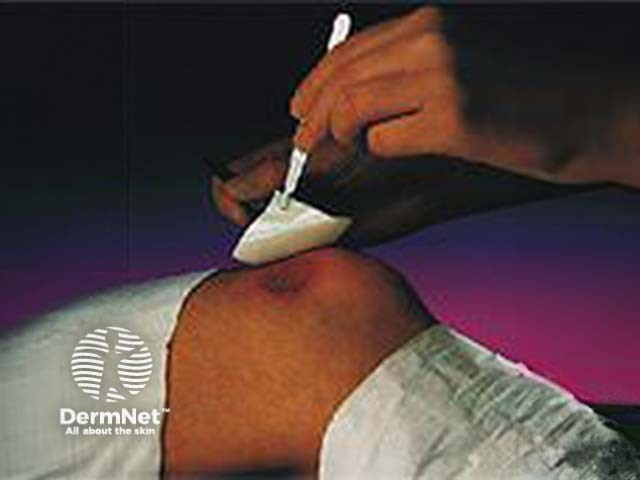

If a wound is discharging fluid (serum), the dressing should be changed often to minimize bacterial growth. After drainage has stopped, there may be no need for a dressing.
Ointments such as petroleum jelly may be applied to limit surface bacterial growth and prevent the dressing from sticking to the wound. Topical antibiotics containing single or multiple antibiotics such as bacitracin, neomycin, or polymyxin B may be useful in a contaminated wound but should be avoided in clean wounds because there is an increasing rate of bacterial resistance to these agents.

Jelonet gauze impregnated with petroleum jelly
Wounds may be cleansed with water, normal saline or with hydrogen peroxide several times daily before the reapplication of ointment.
Use of topical silicone gel sheeting or polyurethane self-adhesive patches after routine dermatologic surgery minimizes the risk of hypertrophic scars and keloids in patients at risk for those lesions.
Dressings designed to reduce scars

Cicacare™ silicone scar dressing
Scar Reduction™ patch polyurethane scar dressing
Dressings for chronic wounds
The principles outlined for acute wounds remain true for chronic wounds including leg ulcers or surgical wounds healing by secondary intention.
In a full-thickness wound, the dermis must be recreated before re-epithelialization can begin. These wounds heal from the base as well as from the edges so the development of some fibrinous exudate in the wound bed is a positive sign.
Occlusive options
Occlusion of chronic wounds:
- Allows macrophages and fibroblasts to enter the wound
- Promotes autolysis mediated by enzymes released from leukocytes.
- Favours cell proliferation because of low pH and hypoxia.
- Enhances growth factors and cytokines within wound fluid.
The occlusive dressings may be divided into five categories:
- Hydrogels
- Hydrocolloid
- Foams
- Films
- Alginates.
Hydrogels are composed primarily of water, fixed in a cross-linked polymer (sodium carboxymethylcellulose, or starch). They may be hydrated or in a dehydrated state requiring moistening with water or saline. They are used to rehydrate dried-out necrotic eschar. Hydrogels are also useful for exudative wounds because they have a high absorptive capacity and are nonadherent. They cool the wound and can provide excellent pain relief. They are also useful for partial thickness wounds from resurfacing procedures and skin graft donor sites.
The hydrogel should be covered by an absorbent layer, made of gauze or cotton, and an outer layer of tape, netting or roll bandage.
Hydrocolloid dressings are a mixture of a hydrophilic base and adhesive, often with an outer covering of polyurethane. They adhere directly to the wound and do not usually require a secondary dressing to keep them in place. In addition, they absorb mild to moderate wound exudate so they can be worn for three to seven days without changing.
Hydrophilic foam dressings are permeable to oxygen and water vapour. They usually have a hydrophobic backing that provides occlusion and some have an adhesive surface, which makes application easier. They can absorb only limited amounts of wound exudate so may need to be changed every two to three days or even more frequently during early wound healing when exudation is greatest.
Foam dressings are ideally suited for superficial and dry wounds eg after ablative resurfacing procedures and chronic ulcers since they provide padding that can relieve pressure over bony prominences.
Thin transparent film dressings are not very absorptive, so they are not useful for wounds with significant exudate. They can be used to keep other dressings in place, including a top layer of an acute surgical wound dressing. They are often used to cover sites of IV insertion, superficial abrasions and as temporary dressings e.g. over local anaesthetic cream prior to venepuncture.
Alginates are highly absorbent and are indicated when a wound is very exudative. They release calcium ions, which help haemostasis so are usefully applied to a surgical wound in a patient with excessive bleeding. In chronic wounds, the exudate combines with the alginate gel to form a green or yellowish goo. The alginates are nonadherent unless the wound dries out. They can be soaked off to avoid unnecessarily debriding the wound.
Dressings for chronic wounds

Curasol™ hydrogel wound dressing

Duoderm™ hydrocolloid dressing

Allevyn™ foam dressing

Opsite™ film dressing

Sorbsan™ alginate dressing
Honey
Honey has been used as a traditional remedy for burns and wounds, and more recently several studies have demonstrated that it has antibacterial activity. Honey can clear an infection from cutaneous wounds and improve healing. Honey from New Zealand manuka (Leptospermum spp) has enhanced antibacterial activity. It is available in a jar (also for oral consumption), a tube, or impregnated on a wound dressing. The antibacterial effect is labelled with its UMF (Unique Manuka Factor) according to Waikato University's honey research unit tests.
Proposed mechanisms include:
- Physicochemical properties (eg, osmotic effects and pH)
- Antiinflammatory activity stimulates immune responses
- Hydrogen peroxide concentration.
Honey for wounds
Active UMF10+ Manuka honey

Medihoney™ wound dressing

Activon™ tulle wound dressing
Choice of dressing
The most suitable dressing depends on the type of wound.
- Necrotic wounds have a dry black eschar composed of dead epidermis
- Sloughy wounds contain yellow viscous adherent slough
- Granulating wounds contain deep red vascularised granulation tissue
- Epithelialising wounds have a pink margin to the wound or isolated pink islands on the surface
- Infected wounds.
It also depends on the location and size of the wound. Some dressings are easier to use and remove than others. Modern dressings are relatively hypoallergenic and non-adherent but sensitisation may occur to iodine, antibiotics, rubber, adhesives and preservatives. A tape cannot be applied if the skin is treated with emollients or topical steroid creams. Cost and availability must also be considered.
Necrotic wounds
The aim is to rehydrate the dry scab so that it will separate off. Options are wet dressings using saline or hypochlorite (Eusol). Hydrogel covered by perforated plastic film absorbent dressing (Melolin or Telfa) or vapour permeable film. Hydrocolloid dressing.
Sloughy wounds
These need debriding to remove the abnormal matrix of fibrin, exudate, inflammatory cells and bacteria. This can be done by surgical debridement or by an agent that soaks up debris and forms a moist gel. Options are:
- Polysaccharide dressing as beads or paste.
- Hydrocolloid dressing if wound less exudative.
- Alginate dressing.
- Enzymes.
Granulating wounds
Granulation tissue is highly vascular matrix of collagen and proteoglycans.
- Cavity wounds are packed with alginate fibre ribbon, silicone foam dressing or foam chips
- Shallow but heavily exuding ulcers are dressed with alginate dressings or hydrophilic foam product
- Less exudative ulcers are dressed with hydrocolloid or thin foam dressing
Epithelialising wounds
Superficial wounds that exude fluid (burns and donor sites):
- Paraffin gauze covered with gauze and cotton tissue (Gamgee)
- Alginate
- Hydrocolloid.
Dry superficial wounds:
- Hydrocolloid
- Film dressing
- Perforated plastic film dressing
- Knitted viscose non-adherent dressings.
Infected wounds
Infected wounds need to be covered because they may have an unpleasant odour, and to prevent the spread of the organisms, particularly if they are resistant to standard antibiotics. Several dressings include antibacterial agents. Their use is controversial.
- Framycetin
- Fusidic acid
- Chlorhexidine
- Povidone-iodine
Bioengineered skin substitutes
Skin autografts are commonly used to cover acute surgical wounds and chronic ulcers. However, harvesting skin grafts create another wound that must heal, and suitable skin is unavailable in some cases such as extensive thermal burns. Sterilised cadaver allografts provide temporary wound dressings but eventually slough off. There has been intensive research and development in recent years to provide a satisfactory substitute for healthy skin. Replacement of dermal matrix and epidermis is required.
Cultured keratinocyte autografts can provide permanent coverage of large area from a skin biopsy. However, 3 weeks are needed for graft cultivation.
Keratinocyte allografts cultured from neonatal foreskins are available immediately. They can be cryopreserved and banked, but are not currently commercially available.
Applying a substitute dermal matrix has been shown to improve the likelihood that cultured epidermal cells (or autologous split skin graft) will take. Several immunologically inert systems are now under investigation for management of refractory venous and diabetic ulcers.

Alloderm™ dermal matrix

Apligraf™ artificial skin in culture
Activity
List the dressings found in your surgery. Describe their use.
Page 6 of 7. Next topic: Wound dressings. Back to: Wound healing contents.
Acknowledgement: many images on these pages have been copied from product-related websites.
References
- Mekkes JR, Loots MAM, van der Wal AC, Bos JD. Causes, investigation and treatment of leg ulceration. Br J Dermatol 2003; 148: 388-401 Medline
- Simon DA, Dix FP, McCollum CN. Clinical review. Management of venous leg ulcers. BMJ 2004;328:1358-1362 (5 June), DOI:10.1136/bmj.328.7452.1358
On DermNet
Information for patients
- Erosions and ulcers
- Leg ulcers
- Pressure ulcers
- Diabetic foot ulcers
- Cutaneous polyarteritis nodosa
- Pyoderma gangrenosum
Other websites
- Medscape Reference:
- Management of venous leg ulcers
- Merck Manual Professional:
