Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Cutaneous infections
Created 2008.
Learning objectives
- Describe terms used in dermatopathology of infections
- Describe the pathological features of selected skin infections and infestations
Introduction
Skin infections may be with bacteria, fungi or viruses. Infestations with parasites are also included in this section. In some of these disorders, histology is a vital part of routine diagnosis particularly when organisms are difficult to identify or culture.
The pathology of the following skin diseases will be outlined:
- Impetigo
- Tuberculosis
- Tinea
- Pityriasis versicolor
- Candidiasis
- Warts
- Herpes
- Molluscum contagiosum
- Scabies
Terminology
Descriptions refer to routine sections stained with haematoxylin and eosin (H&E), unless otherwise specified.
| Subcorneal pustule | Neutrophils clustered just below the stratum corneum |
| Subcorneal blister | Fluid filled cavity just below the stratum corneum |
| Ulceration | Complete epidermal loss |
| Gram-positive | Tissue gram stain reveals organisms e.g. staphylococci, streptococci |
| Gram-negative | Tissue gram stain does not reveal organisms e.g. pseudomonas |
| Acid-fast | Organisms revealed by Ziehl-Neilson, auramine or Fite stain |
| Tuberculoid granuloma | Well-demarcated granuloma surrounded by a lymphocytic infiltrate. |
| Caseation | Cheese-like necrosis of collagen |
| Ballooning degeneration | Enlarged and pale keratinocytes, sometimes with pink intranuclear inclusions, acantholysis or multinucleated keratinocyte formation |
| Molluscum bodies | Eosinophilic to basophilic intracytoplasmic inclusions that push the nucleus and keratohyaline granules aside |
Bacterial infections
The most common bacterial infections of the skin are those caused by streptococci and staphylococci. Tuberculosis is described because it has characteristic granulomatous pathology.
Impetigo
Impetigo is generally recognised by its clinical features and confirmed by culture of gram-positive organisms found on microscopy of a skin swab. However, the histological features of impetigo should be familiar as this infection can be confused with several other skin conditions. Some inflammatory dermatoses and tumours may be secondarily infected with the same organisms as cause impetigo. Link to a clinical description of impetigo.
The histological features of impetigo are:
- Subcorneal pustule
- Pustule may include acantholytic cells
- Sometimes ulceration
- Perivascular mixed infiltrate
- Sometimes gram-positive cocci found in the pustule on tissue gram stain.
Tuberculosis
Cutaneous tuberculosis is uncommon in New Zealand. It has a variety of clinical presentations so the histology is often valuable in diagnosis. Link to a clinical description of cutaneous tuberculosis.
The histological features of tuberculosis are:
- Epidermal hyperkeratosis, papillomatosis, atrophy, acanthosis or ulceration
- Sometimes epidermal neutrophilic microabscesses
- Neutrophil-predominant mixed infiltrate
- Tuberculoid granulomas, sometimes with caseation
- Acid-fast bacilli sometimes present.
Fungal infections
Fungal infections are very common and frequently misdiagnosed as inflammatory skin diseases particularly eczema.
Tinea
Tinea refers to infection with dermatophyte organisms (Microsporum, Trichophyton or Epidermophyton). Link to a clinical description of tinea.
The histological features of tinea are:
- Neutrophils in the stratum corneum
- Mild spongiosis
- Sometimes folliculitis
- Variable mixed inflammatory infiltrate
- Fungal hyphae in stratum corneum or within follicle, best seen with PAS or Grocott stains.
Pityriasis versicolor
Pityriasis versicolor is an infection with Malassezia yeasts. Link to a clinical description of pityriasis versicolor.
The histological features of pityriasis versicolor are:
- Normal-looking skin
- No inflammation
- Hyphae and budding yeast cells in stratum corneum or follicles, best seen with PAS (Periodic Acid-Schiff) or GMS (Gomori Methenamine Silver) stains.
Budding yeasts on skin surface
H&E stain 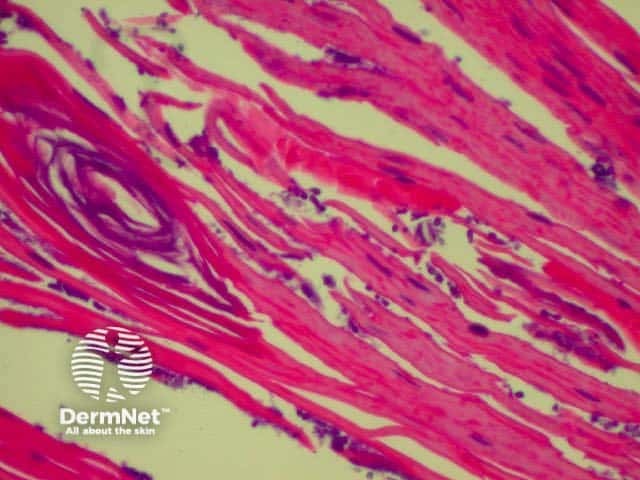
Candidiasis
Candidiasis is due to infection with Candida yeasts. It may have a variety of clinical presentations. Link to clinical descriptions of candida infections.
The histological features of candida infections are:
- Like tinea but with budding yeast cells and pseudohyphae in the stratum corneum
Viral infections
The most common viral infections are papilloma and herpes viruses, and molluscum contagiosum.
Warts
Warts are due to human papillomavirus infection. Link to a clinical description of warts.
The histological features of wart infections are:
- Hyperkeratosis and papillomatosis
- Columns of parakeratosis
- Vacuolated upper keratinocytes with hypergranulosis
- Inwardly sloping rete ridges
- Dilated dermal papillary capillaries
- Perivascular monocyte infiltrate
Herpes
Herpes simplex and herpes varicella zoster infections characteristically result in blistering. Link to clinical descriptions of cold sores, chickenpox and shingles.
The histological features of herpes infections are:
- Intraepidermal vesicle or ulceration
- Epidermal necrosis and ballooning degeneration
- Intranuclear viral inclusions
- Perivascular mixed infiltrate
- Sometimes leukocytoclastic vasculitis
Molluscum contagiosum
Molluscum shows unique histological features and is very easy for a pathologist to diagnose. Link to a clinical description of molluscum contagiosum.
The histological features of molluscum contagiosum are:
- Epidermal hyperplasia
- Crater filled with molluscum bodies (cytoplasmic inclusion bodies)
- Little to dense mixed inflammatory cell infiltration
Parasitic diseases
Scabies
In New Zealand, scabies remains a common cause of severe itching. Link to clinical description of scabies. Skin biopsy is often unhelpful in diagnosis, as on average a patient only has 10 mites and many of the skin lesions are as nonspecific histologically as they are clinically.
The histological features of scabies are:
- Eggs or mites (200-400 microns) present in the subcorneal zone
- Spongiosis &/or epidermal hyperplasia
- Perivascular to diffuse mixed and eosinophil dominant inflammatory infiltrate
Activity
Histopathology is rarely employed to diagnose skin infections. Describe when it may be useful.
References
- Atlas of Dermatopathology. Rapini RP, Jordon RE. Year Book Medical Publishers, Inc. First edition 1998
On DermNet
Information for patients
Books about skin diseases
See the DermNet bookstore.
