Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Synovial sarcoma pathology — extra information
Synovial sarcoma pathology
Author: Adjunct A/Prof Patrick Emanuel, Dermatopathologist, Clinica Ricardo Palma, Lima, Peru. DermNet Editor-in-chief: Adjunct A/Prof Amanda Oakley. June 2018.
Introduction
Histology
Special studies
Differential diagnoses
Introduction
Synovial sarcoma is usually an aggressive deep seated mass presenting around large joints (80% in knee and ankle) in young adults. Rarer superficial cases present in the skin of hands and feet as smaller tumours, which have a more favourable prognosis.
Histology of synovial sarcoma
The histopathology in synovial sarcoma may be biphasic (consisting of spindled and epithelioid cells), monophasic (only spindled cells), or undifferentiated (difficult to recognise without cytogenetic tests). These tumours are usually present in the deep soft tissues but occasionally they are seen in the dermis (figure 1). The spindle cells are arranged in plump fascicles with hyalinization and distinct lobulation (figures 2,3) Biphasic tumours have spindle cells resembling synoviocytes and plump epithelial cells forming glands/cords (figure 4, the epithelioid component is indicated with the arrow).
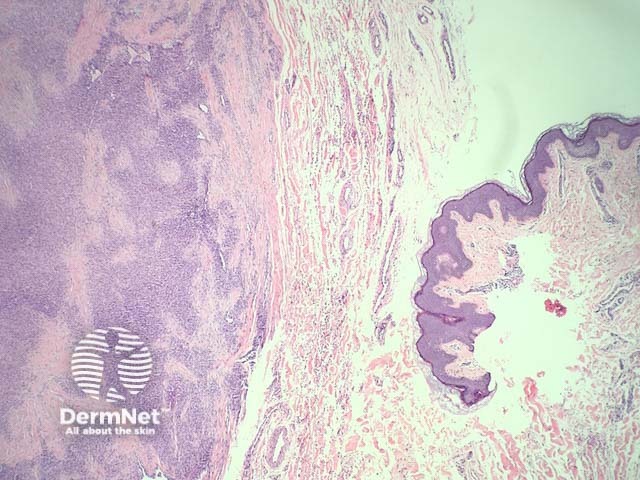
Figure 1
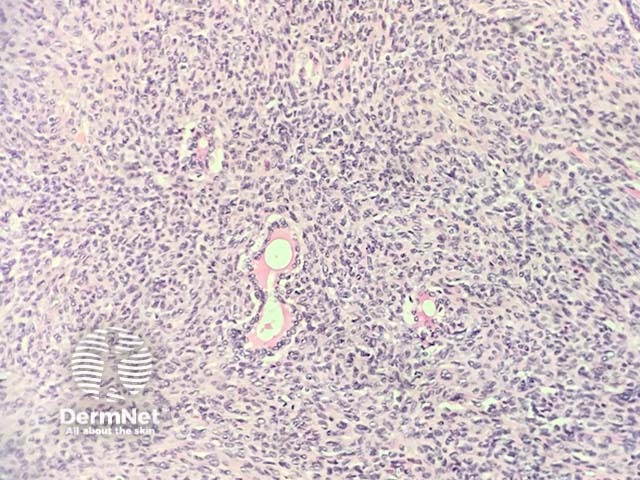
Figure 2
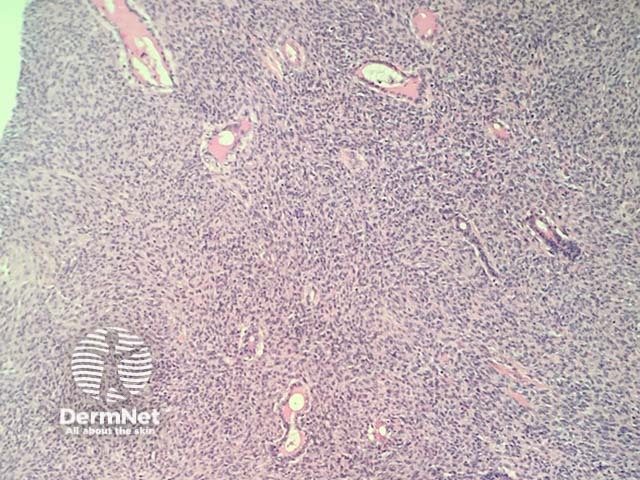
Figure 3
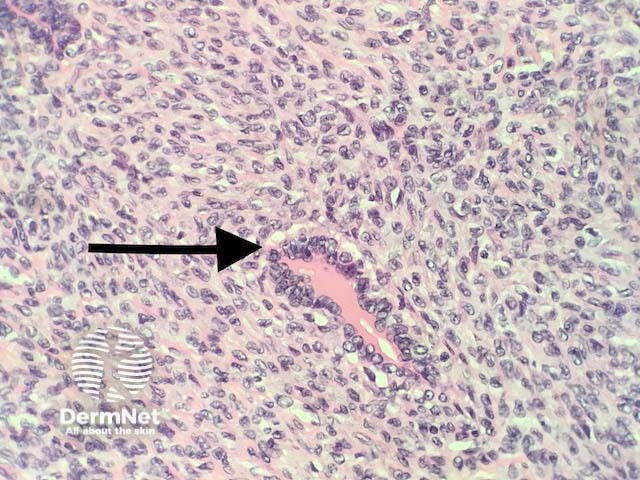
Figure 4
Special studies for synovial sarcoma
Immunohistochemistry reveals the tumour is usually positive with AE1/AE3, EMA, CD99, vimentin, CEA, BCL2.
Cytogenetics are extremely helpful in confirming the diagnosis. A characteristic translocation (t(X;18)(p11.2; q11): SYT-SSX1 or SYT-SSX2 genes) is seen in 90% of cases.
Differential diagnosis for synovial sarcoma
Other sarcomas — monophasic forms of synovial sarcoma can resemble various other sarcomas. A battery of immunohistochemical studies and cytogenetics is almost always needed.
Metastatic adenocarcinoma — the morphology can resemble adenocarcinoma in biphasic sarcoma that has impressive epithelioid areas. The presence of the sarcomatoid areas and ancillary studies can help with the distinction.
Malignant peripheral nerve sheath tumour (MPNST) — these can be particularly difficult to exclude, as some synovial sarcomas are S100 positive (as are MPNST). Ancillary studies are useful for this distinction.
References
- Achtman JC, Pavlidakey PG, Zhang PJ, Elenitsas R, Gutman AB. Synovial sarcoma with cutaneous metastasis. J Cutan Pathol. 2016 Jan;43(1):85–7. PMID: 26332791. PubMed.
On DermNet
Books about skin diseases
