Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Pretibial myxoedema — extra information
Pretibial myxoedema
Author: Dr Kerry Gardner, Dermatology Registrar, Saskatchewan; Copy Editor: Clare Morrison; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand; March 2014. Copy edited by Gus Mitchell.
Introduction Causes Demographics Clinical features Diagnosis Treatment Prognosis
What is pretibial myxoedema?
Pretibial myxoedema is a form of diffuse mucinosis in which there is an accumulation of excess glycosaminoglycans in the dermis and subcutis of the skin. Glycosaminoglycans, also called mucopolysaccharides, are complex carbohydrates that are important for tissue hydration and lubrication. The main glycosaminoglycan in pretibial myxoedema is hyaluronic acid, which is made by cells called fibroblasts.
Pretibial myxoedema is also known as localised myxoedema, thyroid dermopathy, and infiltrative dermopathy.
It is most commonly seen on the shins (pretibial areas) and is characterised by swelling and lumpiness of the lower legs.
What causes pretibial myxoedema?
The exact mechanism for the deposition of glycosaminoglycans in the skin of the lower legs is uncertain.
Pretibial myxoedema is likely to be due to a combination of the following causes.
- An immunological process in which thyroid stimulating hormone receptor (TSH-R) antibodies bind to and stimulate fibroblasts to increase glycosaminoglycan production.
- A cellular process in which fibroblasts are activated indirectly through sensitised T lymphocytes (immune cells). T cells sensitised to a common antigen (likely TSH-R antibodies) could infiltrate dermal tissue and release cytokines (cellular messenger proteins), which activate dermal fibroblasts to produce glycosaminoglycans.
- A mechanical process, where myxoedema accumulates in areas of trauma, after prolonged standing, and in dependent sites. This theory may explain why it occurs in the pretibial area. Dependent swelling could result in pooling of immune cells and proteins, increasing the disease effects.
Who gets pretibial myxoedema?
Pretibial myxoedema is nearly always associated with Graves disease. Graves disease is an autoimmune disorder that affects the thyroid gland in which there are antibodies to TSH-R activate the receptor, often causing an increase in circulating thyroid hormone. This is hyperthyroidism or thyrotoxicosis. Symptoms of thyrotoxicosis include weight loss, palpitations, sweating (hyperhidrosis), and tremors
The classic triad of signs of Graves disease is:
- Pretibial myxoedema
- Ophthalmopathy (prominent eyes due to deposition of myxoedema behind the orbit)
- Acropachy (swelling of distal digits with overgrown nail plates that may lift off the nail bed; similar to clubbing)
Pretibial myxoedema:
- Affects 0.5–4.3% of patients with Graves disease; it is seen in up to 13% in those with severe eye disease
- Has also been seen in patients with Hashimoto thyroiditis, primary hypothyroidism (underactive thyroid), and euthyroidism (normal thyroid function)
- Is associated with high serum concentrations of TSH-R antibodies
- Is most common in people between the ages of 40 and 60
- More commonly affects females, with a female:male ratio of 3.5:1.

Pretibial myxoedema

Thyroid ophthalmopathy

Thyroid acropachy
What are the clinical features of pretibial myxoedema?
Pretibial myxoedema can appear before, during, or after the thyrotoxic state. It is not related to thyroid function. It is generally seen 12–24 months after diagnosis.
- It is most commonly found on the pretibial areas, the dorsum of the feet, or in sites of prior trauma.
- It is usually asymptomatic and more of a cosmetic concern, but can be itchy or sore.
- Early lesions are bilateral, firm, non-pitting, asymmetrical plaques or nodules; they may coalesce to form scaly, thickened and hardened skin areas.
- Hair follicles are often prominent giving a peau d'orange (orange peel) texture.
- The overlying skin may be discoloured, in colours that range from a violet tinge to a slightly pigmented yellow-brown
- There may be localised hyperhidrosis (increased sweating) and/or hypertrichosis (increased hair growth) over the affected skin.

Pretibial myxoedema in Graves disease

Pretibial myxoedema in Graves disease

Pretibial myxoedema in Graves disease
See more images of pretibial myxoedema ...
Types of pretibial myxoedema
The types of pretibial myxoedema can include the following.
- Diffuse, non-pitting oedema (swelling) — the most common form
- Plaque form — raised plaques on a background of non-pitting oedema
- Nodular form — sharply circumscribed tubular or nodular lesions
- Elephantiasic form — nodular lesions with pronounced lymphoedema (swelling due to accumulation of lymphatic tissue fluid). Lesions may coalesce to give the entire extremity an enlarged, warty appearance. This form is rare.
How is pretibial myxoedema diagnosed?
Diagnosis of pretibial myxoedema is made by taking a history and finding characteristic clinical appearance on examination of the patient.
Skin biopsy is rarely necessary for diagnosis, especially if there is a history of hyperthyroidism, or Graves ophthalmopathy.
If a biopsy is done, histopathology typically shows deposition of mucin (glycosaminoglycans) throughout the dermis and subcutis.
Histopathology of pretibial myxoedema
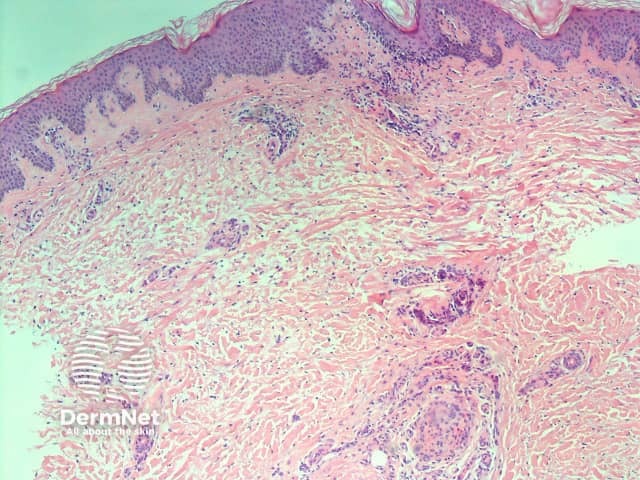
H&E stain
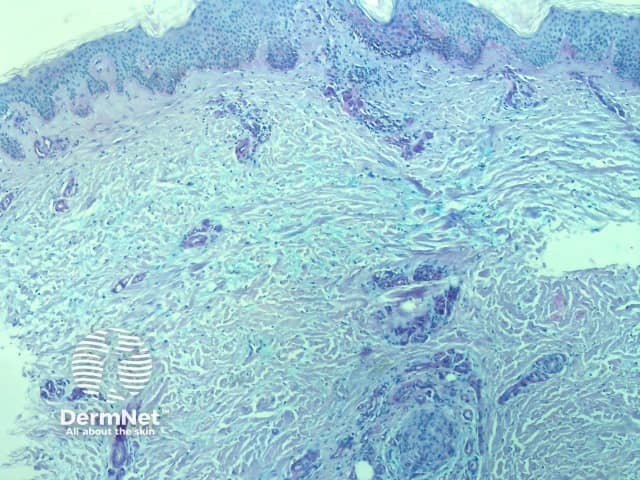
Positive mucin stain
Deposited mucin promotes dermal oedema by promoting the retention of fluid in the skin. This results in compression/occlusion of small peripheral lymphatics and lymphoedema.
The biopsy also shows attenuation of collagen fibres; they may be frayed, fragmented and widely separated. Stellate (star-shaped) fibroblasts are often observed, but the number of fibroblasts remains normal. Often a mild, superficial lymphocytic infiltrate around blood vessels is seen, and the overlying epidermis may show hyperkeratosis (increased scale).
What is the treatment for pretibial myxoedema?
Pretibial myxoedema is often asymptomatic and mild, and may require no treatment at all.
If symptomatic, treatment options include:
- Minimisation of risk factors
- Avoid tobacco
- Reduce weight
- Normalise thyroid function
- Compression stockings, which can be worn to improve lymphoedema
- Mid to high potency topical corticosteroid, which are usually recommended under occlusion (eg, plastic cling-film wrap) nightly or every other night to enhance effect.
Other therapies reported to be successful include:
- Intralesional corticosteroids
- Systemic steroids
- Pentoxifylline
- Octreotide
- Rituximab
- Plasmapheresis
- Intravenous immunoglobulin
- Teprotumumab
- Surgical excision has been successful in case reports, but it is generally not recommended due to the risk of pretibial myxoedema developing in injured skin.
What is the prognosis for pretibial myxoedema?
The prognosis is generally quite good. Most patients with asymptomatic pretibial myxoedema do not require treatment or follow-up.
The myxoedema clears up completely in the majority of patients with mild disease.
Even with more severe disease, it resolves in more than half of patients after several years. The elephantiasic form is the most difficult to treat, and is the least likely to clear up.
The likelihood of remission depends on the severity of the initial disease rather than its treatment.
References
- Anderson CK, Miller OF 3rd. Triad of exophthalmos, pretibial myxedema, and acropachy in a patient with Graves' disease. J Am Acad Dermatol 2003; 48: 970–2. DOI: 10.1067/mjd.2003.323. PubMed
- Antonelli A, Navarranne A, Palla R, Alberti B, Saracino A, Mestre C, Roger P, Agostini S, Baschieri L. Pretibial myxedema and high-dose intravenous immunoglobulin treatment. Thyroid 1994; 4: 399–408. DOI: 10.1089/thy.1994.4.399. PubMed
- Eds; Bolognia, JL, Jorizzo, JL, Rapini, PR. Dermatology: 3rd Edition. 2012. Mosby.
- Daumerie, C, Ludgate, M, Costagliola, S, Many, MC. Evidence for thyrotropin receptor immunoreactivity in pretibial connective tissue from patients with thyroid-associated dermopathy. Eur J Endocrinol 2002; 146: 35–8. DOI: 10.1530/eje.0.1460035. PubMed
- Chief Ed: Elder, D; Eds: Elenitsas R, Johnson BL Jr, Murphy GF, Xu G. Lever’s Histopathology of the Skin: 10th Edition. 2008. Lippincott Williams & Wilkins.
- Engin B, Gümüşel M, Ozdemir M, Cakir M. Successful combined pentoxifylline and intralesional triamcinolone acetonide treatment of severe pretibial myxoedema. Dermatol Online J 2007; 13: 16. PubMed
- Fatourechi V. Pretibial myxoedema: pathophysiology and treatment options. Am J Clin Dermatology 2005; 6: 295–309. doi: 10.2165/00128071-200506050-00003. PubMed
- Fatourechi V, Pajouhi M, Fransway AF. Dermopathy of Graves disease (pretibial myxoedema). Review of 150 cases. Medicine (Baltimore) 1994; 73: 1. doi: 10.1097/00005792-199401000-00001. PubMed
- Heyes C, Nolan R, Leahy M, Gebauer K. Treatment-resistant elephantiasic thyroid dermopathy responding to rituximab and plasmapheresis. Australas J Dermatol 2012; 53: e1. doi: 10.1111/j.1440-0960.2010.00693.x. PubMed
- Jolles S, Hughes B. Use of IGIV in the treatment of atopic dermatitis, urticaria, scleromyxoedema, pyoderma gangrenosum, psoriasis, and pretibial myxoedema. International Immunopharmacology 2006; 579–91. DOI: doi.org/10.1016/j.intimp.2005.11.017. Journal
- Mitchell AL, Gan EH, Morris M, Johnson K, Neoh C, Dickinson AJ, Perros P, Pearce SH. The effect of B cell depletion therapy on anti-TSH receptor antibodies and clinical outcome in glucocorticoid-refractory Graves' orbitopathy. Clin Endocrinol (Oxf) 2013; 79: 437–42. doi: 10.1111/cen.12141. PubMed
- Pineda AM, Tianco EA, Tan JB, Casintahan FA, Beloso MB. Oral pentoxifylline and topical clobetasol propionate ointment in the treatment of pretibial myxoedema, with concomitant improvement of Graves' ophthalmopathy. J Eur Acad Dermatol Venereol 2007; 21: 1441–3. doi: 10.1111/j.1468-3083.2007.02259.x. PubMed
- Schwartz KM, Fatourechi V, Ahmed DD, Pond GR. Dermopathy of Graves' disease (pretibial myxoedema): long-term outcome. J Clin Endocrinol Metab 2002; 87: 438. doi: 10.1210/jcem.87.2.8220. PubMed
- Türke B, Balázs C. [Treatment of pretibial myxoedema with pentoxifylline]. Orv Hetil 2012; 153: 1719–22. doi: 10.1556/OH.2012.29472. PubMed
- Gill RS. Pretibial myxoedema. Available from: https://emedicine.medscape.com/article/1103765-overview (accessed March 2014).
- Weedon, D. Weedon’s Skin Pathology: 3rd Edition. 2010. Elsevier.
- Eds: Wolff K, Goldsmith LA, Katz SI, Gilchrist BA, Paller AS, Leffell DJ. Fitzpatrick’s Dermatology in General Medicine: 7th Edition. 2008. McGraw-Hill.
On DermNet
- Thyroid disease
- Mucinoses
- Plasmapheresis for skin disease
- Remitting seronegative symmetrical synovitis with pitting oedema
Other websites
- Pretibial myxoedema — Medscape Reference
