Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Naevus simplex — extra information
Naevus simplex
Author: Wei Wu, Medical Student, The University of Auckland, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. January 2019.
Introduction Demographics Causes Clinical features Diagnosis Differential diagnoses Treatment and Outcome
What is naevus simplex?
Naevus simplex is a common, benign capillary vascular malformation. It presents at birth as a pink or red patch and is most often observed on the nape of the neck, eyelid, or glabella [1,2].
Naevus simplex is also called:
- Salmon patch
- Stork bite (when on the nape of the neck)
- Angel’s kiss (when on the glabella and eyelids)
- Naevus flammeus simplex.
Naevus simplex — the stork mark

Naevus simplex
Naevus simplex

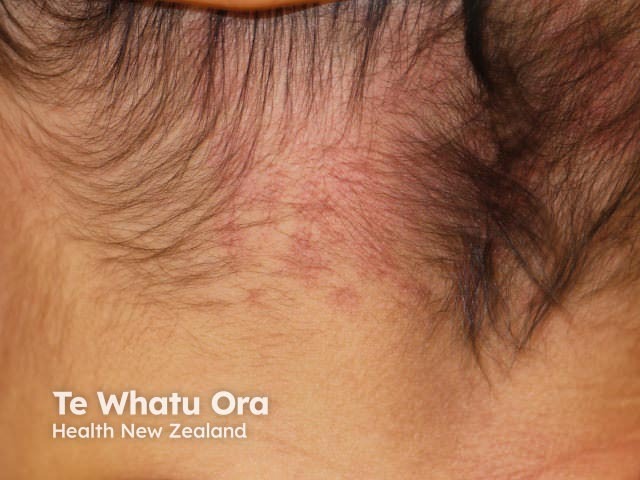
Adult naevus simplex
Who gets naevus simplex?
Naevus simplex affects infants of all races; it occurs in approximately 40% of Caucasian infants and less often in darker-skinned infants [1,3]. It affects male and female infants equally [4].
What causes naevus simplex?
Naevus simplex results from a delay in the maturation of skin cells during embryonic development, following the migration and fusion of cells in the skin nervous system (the neuroectoderm). This results in the characteristic dilation of the dermal capillaries that defines the naevus simplex skin patch. Reduced regulation by autonomic nerves may be a contributing factor in cases of naevus simplex [2,3].
What are the clinical features of naevus simplex?
Naevus simplex is present at birth as either single or multiple, flat, pink or red patches, typically occurring with an indistinct, irregular border and blanching on compression [1,2]. Naevus simplex becomes more red with crying, fevers, breath holding, straining, vigorous physical activity, and changes in ambient temperature [1,2,5]. They tend to become less prominent as the child gets older.
The skin lesions usually occur at midline [4] and can be bilateral and symmetrical in presentation [6]. They are most commonly found on the nape of the neck, eyelids, and glabella, but they may also involve the forehead, scalp, nose, lips, and back [1,2]. Naevus simplex is not painful or itchy [7].
The term ‘naevus simplex complex’ has been proposed for widespread lesions occurring beyond the common sites [2].
Disease associations with naevus simplex
Midline lumbosacral naevus simplex is sometimes called a ‘butterfly-shaped mark’ and is occasionally observed in a baby with spinal dysraphism. Imaging studies that look for spinal dysraphism (abnormal fusion of the neural tube) may be undertaken if there are other local skin changes such as excess hair growth (localised hypertrichosis), a dermal sinus or pit, a lipoma, or a deviated gluteal cleft, or many similar lesions elsewhere. Infants with a naevus simplex at the lumbosacral midline often also have other similar lesions appearing elsewhere [2,4].
Naevus simplex is occasionally observed in a baby with another condition, such as:
- Beckwith–Wiedemann syndrome [2]
- Macrocephaly-capillary malformation syndrome [2]
- Odontodysplasia [2]
- Nova syndrome [2]
- Roberts syndrome [2]
- Rubinstein–Taybi syndrome [1].
It is uncertain whether there is a true association of naevus simplex with these syndromes [1,4].
How is naevus simplex diagnosed?
Naevus simplex can be diagnosed by its clinical appearance and no further testing is usually required [7].
What is the differential diagnosis for naevus simplex?
Naevus simplex is sometimes confused with naevus flammeus (port wine stain) or with infantile haemangioma (strawberry naevus) because these vascular lesions are also seen in infants.
Naevus flammeus
Naevus flammeus is a capillary vascular malformation found in 0.3% of newborn infants [1,6]. The lesions present as pink, red or purple patches and can be localised, extensive or multiple [1,6]. Unlike naevus simplex, naevus flammeus tends to be unilateral, often persisting, darkening and thickening with increasing age [1,6].
Infantile haemangioma
Infantile haemangioma is a vascular tumour found in 1.1–2.6% of newborn babies, and it occurs in 10% of infants by 1 year of age. It affects female infants more often than males. The haemangioma begins as a pink patch and then enlarges. It is most commonly found on the head and neck of an infant but may also arise on other body sites. Infantile haemangioma usually resolves after infancy, but it can leave a residual mark [1,6].
Vascular lesions in infants

Naevus simplex

Naevus flammeus

Infantile haemangioma
What is the treatment and outcome for naevus simplex?
On most body sites, naevus simplex fades and disappears within the first 1–2 years of life [2]. A lesion on the nape of the neck fades more slowly and incompletely, and it has a 50% chance of persisting indefinitely [1,5]. As this site is often covered by hair, it may not be a cosmetic issue.
Pulsed dye laser therapy could be considered to lighten the colour of a persistent lesion [6].
References
- Freedberg I, Eisen A, Wolff K, Austen K, Goldsmith L, Katz S (eds). Fitzpatrick's dermatology in general medicine, 6th edn. New York: McGraw-Hill, 2003.
- Juern A, Glick Z, Drolet B, Frieden I. Nevus simplex: A reconsideration of nomenclature, sites of involvement, and disease associations. J American Academy of Dermatology. 2010; 63: 805–14. DOI: 10.1016/j.jaad.2009.08.066. PubMed
- Leung A, Telmesani A. Salmon patches in Caucasian children. Pediatr Dermatol 1989; 6: 185–7. PubMed.
- Eichenfield L, Frieden I, Zaenglein A, Mathes E (eds). Neonatal and infant dermatology, 3rd edn. Philadelphia: Elsevier, 2014.
- Cohen B. Hemangiomas in infancy and childhood. Pediatr Ann 1987; 16: 17–26. PubMed
- McLaughlin M, O’Connor NR, Ham P. Newborn skin: Part II. Birthmarks. Am Fam Physician 2008; 77: 56–60. PubMed
- Skinsight. Salmon Patch. 2018. Available at: www.skinsight.com/skin-conditions/infant/salmon-patch (accessed 19 March 2018).
On DermNet
- Capillary vascular malformation
- Congenital naevi
- Vascular proliferations and abnormalities of blood vessels
- Vascular skin problems
