Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Mucosal melanoma — extra information
Mucosal melanoma
Author: Debra Yeh, Medical Student, University of Auckland, New Zealand; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, April 2014.
Introduction Common sites Demographics Causes Signs and symptoms Tests Staging Treatment Prognosis
What is mucosal melanoma?
Melanoma develops if there is uncontrolled growth of melanocytes, the cells responsible for pigmentation. The majority of melanomas are cutaneous, ie they grow within the skin.
Mucosal melanoma is a rare type of melanoma that occurs on mucosal surfaces. Mucous membranes are moist surfaces that line cavities within the body. This means that mucosal melanoma can be found in the respiratory tract, gastrointestinal tract or genitourinary tract.
Mucosal melanomas are most often found in the head and neck, in the eyes, mouth, nasopharynx and larynx, but they can also arise throughout the gastrointestinal tract, anus and vagina. They make up approximately 1.1% of all melanomas but are usually more complicated because of late diagnosis due to their less visible locations and because they are often amelanotic – meaning they are not pigmented.
Which parts of the body are affected by mucosal melanoma?
Subtypes of mucosal melanoma are based on the tissue in which they arise. Melanoma can start within any mucosal epithelium. The most common sites are:
- Respiratory tract
- Nasal cavity
- Paranasal sinuses
- Oral cavity
- Gastrointestinal tract
- Transitional zone of anal canal (the line where the normal skin meets the mucous membrane)
- Genitourinary tract
- Vulva
- Vagina
Who gets mucosal melanoma?
The peak age of diagnosis of mucosal melanoma is between 70 and 79. However, younger people have also been known to develop mucosal melanoma, especially of the oral cavity.
Mucosal melanoma of the genital tract is more common in females.
What causes mucosal melanoma?
While there are many suggested risk factors for mucosal melanoma, there is only weak evidence for all, and none that are widely accepted. About 25% of mucosal melanomas have been linked with problems with a gene called KIT. Genes are the templates used for making protein, and mutations in the KIT gene cause the production of a mutant protein. The KIT gene can also be over-expressed, which means that there is more of the KIT protein being made than usual. Both the mutation and over-expression of the KIT gene have been associated with mucosal melanoma.
Possible risk factors include:
Oral mucosal melanoma
- Smoking
- Ill-fitting dentures
- Ingested/inhaled environmental carcinogens
Vulvar melanoma
- Chronic inflammatory disease
- Viral infections
- Chemical irritants
- Genetic factors
Anorectal melanoma
Signs and symptoms of mucosal melanoma
The signs and symptoms of mucosal melanoma largely depend on its location. Therefore, there are a wide variety of symptoms that patients may experience.
Mucosal melanoma of the head and neck
- Discolouration in the mouth
- Painless bleeding lump
- Ulceration
- Ill-fitting dentures
- Nasal obstruction
- Nose bleeds
- Loss of smell
Vulvovaginal melanoma
- Discolouration of the vulva
- Itch
- Bleeding
- Discharge
- Ulceration
- A mass
- Pain during/after intercourse
Anorectal melanoma
- Bleeding
- A mass
- Anal or rectal pain
- Change in bowel habit (such as constipation or diarrhoea)
What testing is done in mucosal melanoma?
If there is suspicion of mucosal melanoma, the most important test is a biopsy of the involved tissue. If the pathology report indicates melanoma, the patient will be fully examined and further tests may be undertaken to find out if it has spread further. These may include:
- Biopsy of the mucosal melanoma
- CT and/or MRI to assess the primary site of disease
- CT and/or PET scan to assess for metastases and lymph node involvement
Staging of mucosal melanoma
Head and neck mucosal melanoma
The American Joint Committee on Cancer (AJCC) Tumour, Node, and Metastasis (TNM) classification is used to stage mucosal melanoma of the head and neck. Mucosal tumour staging begins at T3 (advanced). Like cutaneous melanoma, mucosal melanoma can also spread to lymph nodes or through the blood stream to other areas of the body. Here, they can form new tumours. These are referred to as metastases.
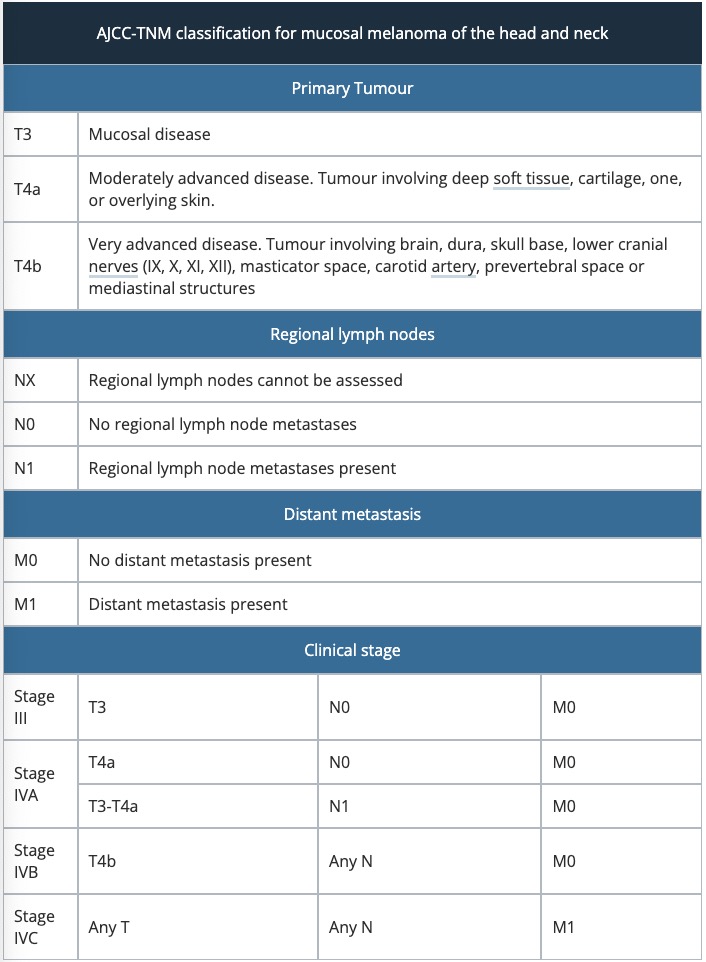
Vulvovaginal mucosal melanoma
Vulval melanomas are staged using the same AJCC-TNM classification as the table above. There is no staging system for vaginal melanoma, so a simplified clinical staging system can be used to categorise these melanomas.
Stage I |
Clinically localised disease |
||
Stage II |
Regional nodal involvement |
||
Stage III |
Distant metastatic involvement |
||
Anorectal mucosal melanoma
Anorectal mucosal melanoma is staged using the same simplified staging system as vaginal melanoma.
Stage I |
Clinically localised disease |
||
Stage II |
Regional nodal involvement |
||
Stage III |
Distant metastatic involvement |
||
Treatment of mucosal melanoma
The best form of treatment for mucosal melanoma is wide local excision of the lesion. This may not always be possible, as the melanoma may be located on an important anatomical structure, or be too large to excise safely.
Due to the likelihood of the same melanoma recurring, surgical resection is often combined with radiotherapy. Radiotherapy is also a consideration for patients who are not suitable for surgery.
Prognosis of mucosal melanoma
Mucosal melanomas have a poor prognosis, as most patients develop metastases despite aggressive therapy.
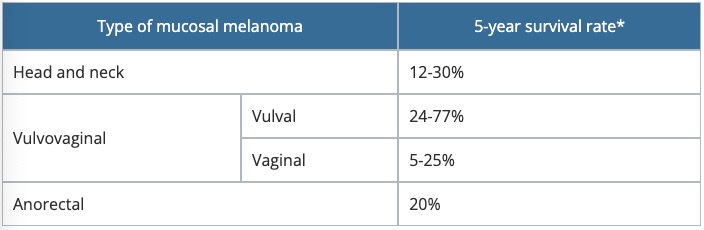
*The 5-year survival rate refers to the percentage of patients that survive for at least 5 years after their diagnosis, and is approximate.
References
- Tacastacas JD, Bray J, Cohen YK, Arbesman J, Kim J, Koon HB, Honda K, Cooper KD, Gerstenblith MR. Update on primary mucosal melanoma. J Am Acad Dermatol. 2014 May 6. pii: S0190-9622(14)01265-1. PubMed
- Bishop KD, Olszewski AJ. Epidemiology and survival outcomes of ocular and mucosal melanomas: a population-based analysis. International Journal of Cancer. 2013: n/a-n/a. PubMed
- Meleti M, Leemans CR, Mooi WJ, Vescovi P, van der Waal I. Oral malignant melanoma: a review of the literature. Oral Oncology. 2007; 43: 116–21. Journal
- Mihajlovic M, Vlajkovic S, Jovanovic P, Stefanovic V. Primary mucosal melanomas: a comprehensive review. International Journal of Clinical and Experimental Pathology. 2012; 5: 739. PubMed Central
- Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. Journal of the American Academy of Dermatology. 2007; 56: 828–34. PubMed
- Vikey AK, Vikey D. Primary malignant melanoma, of head and neck: A comprehensive review of literature. Oral Oncology. 2012; 48: 399–403. PubMed
On DermNet
Other websites
- Mucosal Melanoma — Melanoma.org reference
- TNM Classification for Mucosal Melanoma of Head and Neck — Medscape reference
- Mucosal Melanoma — UpToDate (for subscribers)
- Melanoma risk assessment tool — Melanoma Institute of Australia
- Melanoma education — Melanoma Institute of Australia
