Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Microgeodic disease — extra information
Microgeodic disease
Author: Dr Anne Davis, Dermatologist, Christchurch, New Zealand, 2013.
Introduction Demographics Clinical features Diagnosis Complications Treatment
What is microgeodic disease?
A geode is defined as a small hollow rock. The term microgeodic was coined by a French radiologist Maroteaux to describe the x-ray finding of very small (< 1mm) punched out lacunar-like osteolytic lesions (radiographic holes) in the small bones of the fingers of infants affected by this condition [1].
Microgeodic disease or syndrome is rare. In most cases, it is thought to be due to cold-induced vasospasm, which results in avascular necrosis (self-destruction) of the bone. It is also called transient phalangeal osteolysis.
Who gets microgeodic disease?
Microgeodic disease occurs in children. It was first reported in infants but has been reported to occur in children up to the age of 16, with an average age of 7 years. The majority of reported cases have come from Japan [2].
What are the clinical features of microgeodic disease?
Microgeodic disease usually occurs in the winter months. Patients present with swelling of one or more fingers or toes. There may be redness and sometimes pain. Often the clinical changes are described as 'chilblain-like' although chilblains have rarely been reported in association with microgeodic disease [3,4].
The hands are more commonly affected than the toes. Most often only one digit is affected, most frequently the index and middle fingers. The middle phalanx is most commonly affected and the distal phalanx rarely affected [2].
Most cases resolve spontaneously within six months although some cases have taken several years to resolve [2].

Swollen finger originally diagnosed as chilblains

Persistent swelling middle phalanx index finger
How is the diagnosis of microgeodic disease made?
The diagnosis is often made clinically.
Routine blood tests generally show no abnormalities. Inflammatory markers are usually normal.
An x-ray of the affected digit shows small lucent spaces or 'microgeodes'. These are small osteolytic areas with a sclerotic lining. There may be a periosteal reaction.
The differential diagnosis of osteolytic lesions includes tuberculosis, osteomyelitis, sarcoidosis, sickle cell anaemia and neoplasms.
The x-ray findings are localised to the affected phalanx (or phalanges when multiple digits are affected). In contrast, MRI has been reported to show bone marrow oedema in many phalanges of the affected hand, where clinical and radiological findings are absent [5,6].

X-ray
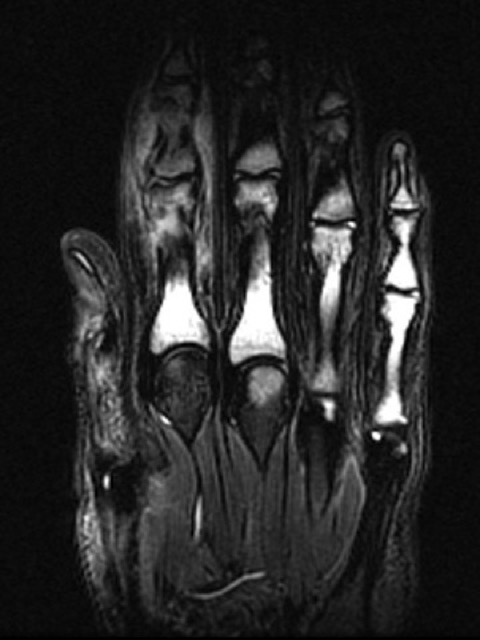
MRI
A biopsy of the affected bone shows necrosis of bone and fibrosis (scarring). Skin biopsy has rarely been performed in microgeodic disease. When concomitant chilblains have been suspected, skin biopsy has shown a lymphocytic vasculitis consistent with this diagnosis.
What are the complications of microgeodic disease?
In a small number of cases, microgeodic disease has been complicated by pathological fracture, which may heal with angulation deformity of the digit. Also, the affected phalanx has been reported to be shortened, suggesting the involvement of the growth plate.
What is the treatment for microgeodic disease?
As microgeodic disease is thought to be due to exposure to cold, it is important to keep the affected limb warm and dry.
If bone changes are severe, it may be worthwhile splinting the finger to prevent fracture.
Vasodilators such as calcium channel blockers have been used to treat chilblains and can be a possible treatment option for microgeodic disease
References
- Maroteaux P. Cinq observations d’une affection microgeodique des phalanges du nourisson d’etiologie inconnue. Ann Radiol (Paris) 1970; 13: 229–36
- Inoue G, Miura T. Microgeodic disease affecting the hands and feet of children. J Pediatr Orthop. 1991 Jan-Feb;11(1):59–63. doi: 10.1097/01241398-199101000-00012. PubMed.
- Prindaville B, Antaya RJ. Chilblains and microgeodic disease diagnosed concurrently in a child's toe. Pediatr Dermatol. 2013 Mar-Apr;30(2):269–70. doi: 10.1111/j.1525-1470.2011.01665.x. Epub 2012 Jan 26. PubMed.
- Davis A, Sew Hoy M. Microgeodic disease and concurrent Chilblains. A case report. Abstract. NZDSI Annual Conference July 2013
- Fujita A, Sugimoto H, Kikkawa I, Hyodoh K, Furuse M, Hoshino Y. Phalangeal microgeodic syndrome: findings on MR imaging. AJR Am J Roentgenol. 1999 Sep;173(3):711–2. doi: 10.2214/ajr.173.3.10470909. PubMed.
- Lee RK, Griffith JF, Read JW, Ng AW, Bellemore M. Phalangeal microgeodic disease: report of two cases and review of imaging. Skeletal Radiol. 2013 Mar;42(3):451–5. doi: 10.1007/s00256-012-1561-8. Epub 2013 Jan 8. PubMed.
On DermNet
