Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Metastatic Crohn disease pathology — extra information
Systemic diseases Autoimmune/autoinflammatory
Metastatic Crohn disease pathology
Author: Harriet Cheng BHB, MBChB, Department of Dermatology, Waikato Hospital, Hamilton, New Zealand; A/Prof Patrick Emanuel, Dermatopathologist, Auckland, New Zealand, 2013.
Crohn disease patients may develop sterile granulomatous skin lesions at sites removed from the gastrointestinal tract This is known as metastatic Crohn disease (MCD). When it affects the skin, it is also called cutaneous Crohn disease. Clinically, MCD presents as a solitary or multiple nodules, plaques, ulcers, lichenoid lesions, or violaceous perifollicular papules.
Histology of metastatic Crohn disease
Metastatic Crohn disease is characterised by a dermal granulomatous infiltrate composed of epithelioid histiocytes (figures 1-5). There is an associated infiltrate which is mainly lymphocytic but may be rich in eosinophils. The granulomas may encroach on the epidermis (figure 1). Massive oedema may be seen (figure 2). Ulceration of the overlying epidermis is a common feature (figure 4).
Granulomatous vasculitis and necrosis may also be seen in metastatic Crohn disease.
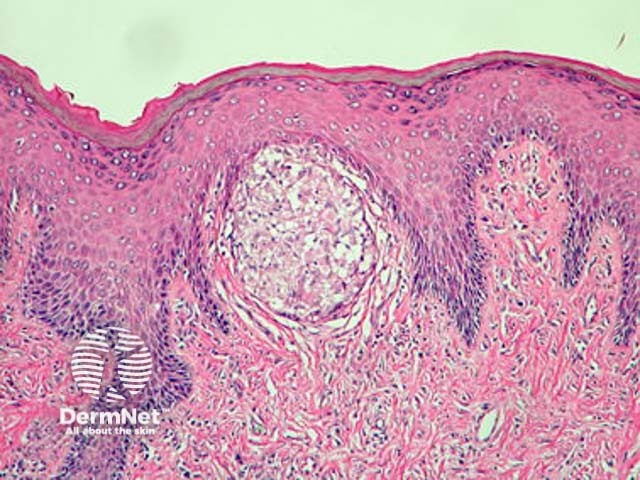
Figure 1
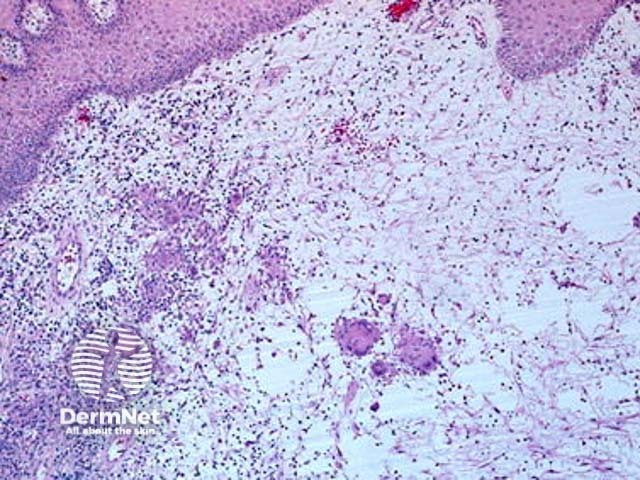
Figure 2
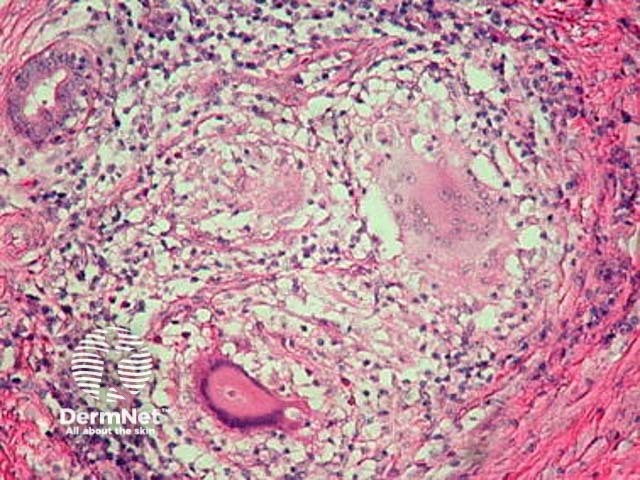
Figure 3
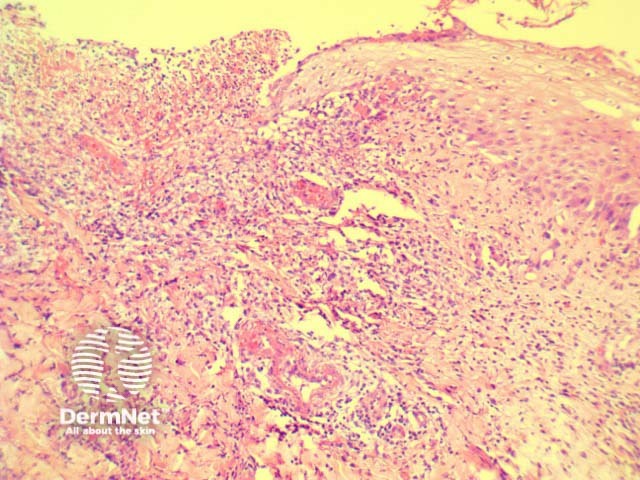
Figure 4
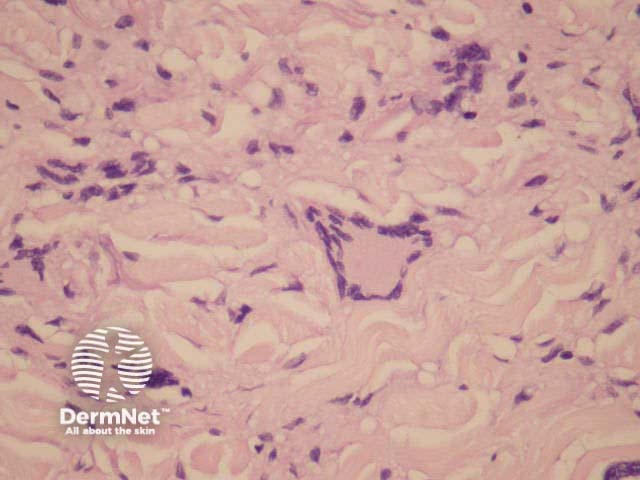
Figure 5
Differential diagnosis of metastatic Crohn disease
Sarcoidosis: This may be a very difficult distinction without clinical correlation. Granulomata of Crohn disease are frequently less well-defined (figure 5) than in sarcoidosis. Ulceration is less common in sarcoidosis. Eosinophils are less dense in sarcoidosis.
Mycobacterial infection: Special stains and culture are required to exclude mycobacterial infection.
Granulomatous cheilitis (orofacial granulomatosis): This condition may be histologically identical. Clinical features help to differentiate.
References
- Emanuel PO, Phelps RG. Metastatic Crohn's disease: a histopathologic study of 12 cases. J Cutan Pathol. 2008 May;35(5):457-61.
On DermNet
