Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Melanocytic lesions pathology — extra information
Lesions (cancerous) Diagnosis and testing
Melanocytic lesions pathology
Author: A/Prof Patrick Emanuel, Dermatopathologist, Auckland, New Zealand; Harriet Cheng BHB, MBChB, Dermatology Department, Waikato Hospital, Hamilton, New Zealand, 2013.
This may be confusing for the clinician, but in ambiguous cases open communication with your pathologist by email or telephone is invaluable. As always, supplying the pathologist with adequate clinical details including a detailed description of the lesion is essential for accurate diagnosis. Ideally, send clinical images with your specimens, but diagrams showing areas of concern are also useful. Many pathologists now welcome dermatoscopic images.
Practical pathologic approach to primary melanocytic lesions
The inexperienced pathologist should:
-
Try to glean as much clinical information as possible. Clinical and dermatoscopic images can be very helpful.
-
Ensure the laboratory staff are skilled in embedding and cutting skin specimens.
-
Examine the entire melanocytic lesion histopathologically.
-
Examine at least 3 levels histopathologically.
-
If the diagnosis is clear, finalise the case. Melanomas should be reported synoptically.
-
If the diagnosis is not clear, perform immunohistochemistry.
-
If still uncertain consult a colleague/s.
-
If colleague also uncertain, consider molecular tests.
-
If molecular tests not available/unhelpful, be honest and convey the problem to the clinician, i.e. diagnose it as a Diagnostically Ambiguous Melanocytic Neoplasm (DAMN). Consider recommending surgical excision parameters appropriate for melanoma without sentinel lymph node biopsy.
Special stains for melanocytes
Special stains can be used to confirm melanocytic origin in lesions with spindle or epithelioid morphology.
Immunohistochemical stains for melanocytes:
- Human melanoma black (HMB-45): HMB-45 is often diffusely positive in melanoma; zonal staining, in which there is diminished staining in deeper parts of the lesion, is more suggestive, but in no way diagnostic, of a naevus (figures 1, 2) HMB-45 is usually negative in desmoplastic melanoma.
- MART-1 (Melan-A): this highlights every melanocyte so is an excellent means of assessing pagetoid spread, margins and extent of the lesion (figures 3, 4). It is less sensitive in spindled and desmoplastic melanoma.
- S-100 protein: Very sensitive. S-100 is useful if you are not sure if the tumour is melanocytic or another cell type (figure 5)
- Sry-related HMG-BOX gene 10 (SOX10): a nuclear stain for melanocytes and schwannian cells. It is less likely to be expressed by background fibrocytes and histiocytes than S-100. Excellent choice if you are not sure if the tumour is melanocytic or another cell type.
- Ki-67 (MIB-1): this may be useful in distinguishing benign melanocytic naevi (where less than 5% of melanocytes are positive) from melanoma (more than 25% are positive). These percentages are rough guidelines and by no measure absolutely diagnostic. Because assessing the percentage is so subjective and counting positive cells is so tedious, computer software has evolved to aid in this assessment (figure 6).
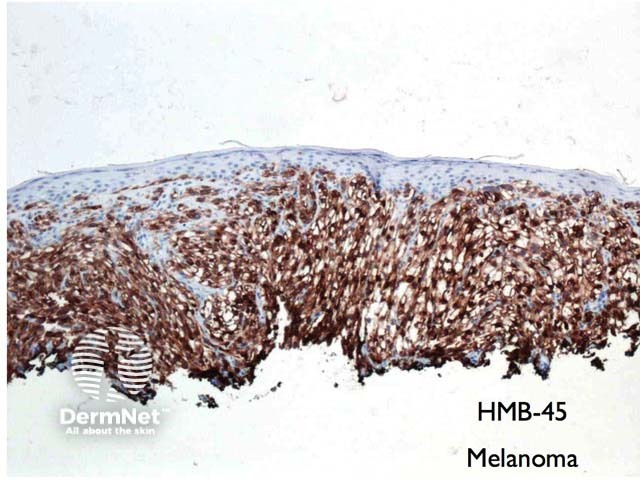
Figure 1
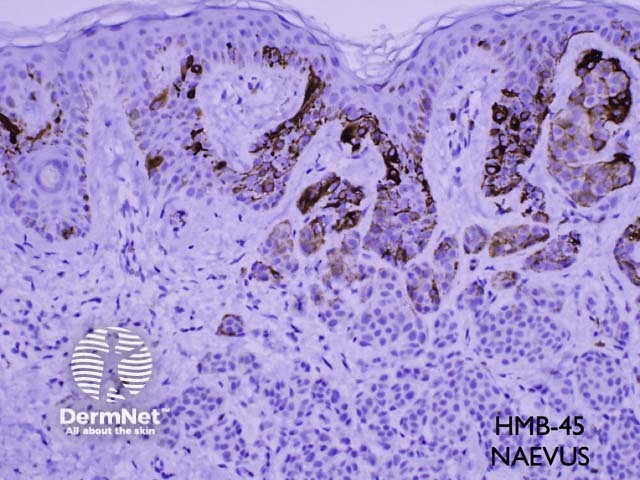
Figure 2
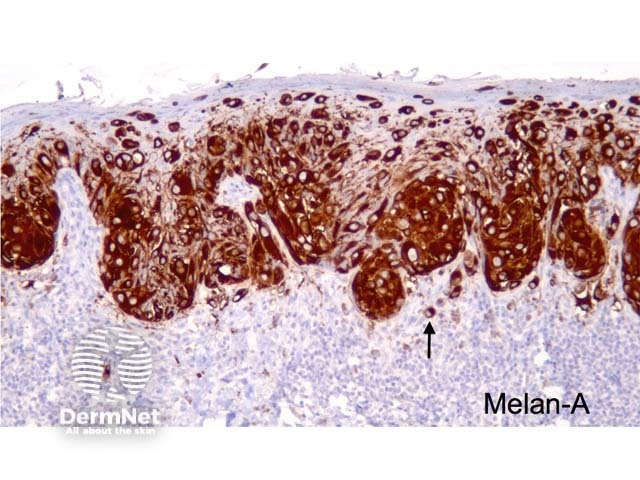
Figure 3
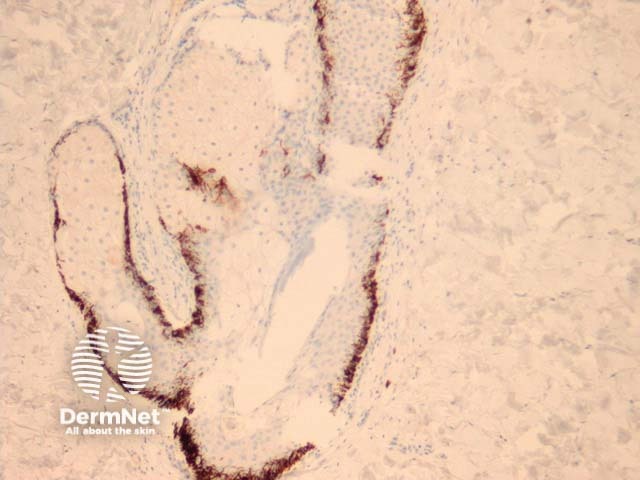
Figure 4
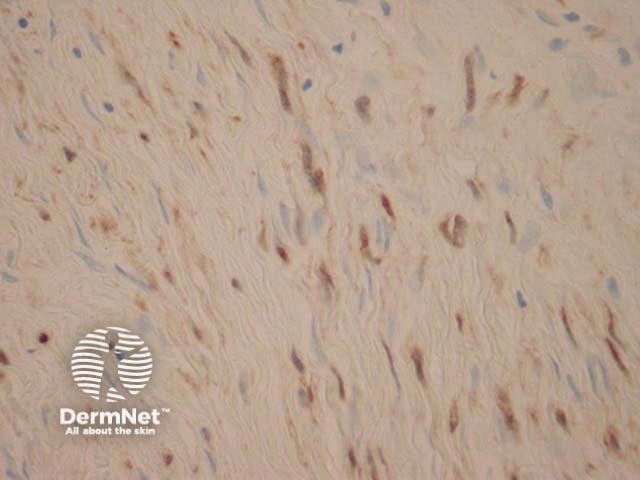
Figure 5
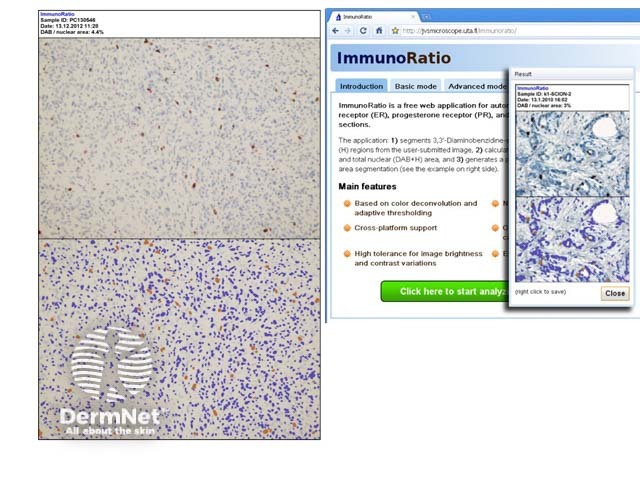
Figure 6
References
- LEVER'S HISTOPATHOLOGY OF THE SKIN. David Elder, MB, CHB, FRCPA. Publisher: Lippincott Williams & Wilkins. Publication Date: 2009
On DermNet
