Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lipodystrophy — extra information
Lipodystrophy
Author: Dr Paul Jarrett, Dermatologist, Tauranga, New Zealand, 2005; Updated: Dr Shawn Jordan, House Officer, North Shore Hospital, Auckland, New Zealand; Hon Assoc Prof Paul Jarrett, Dermatologist, Middlemore Hospital and Department of Medicine, The University of Auckland, Auckland, New Zealand. Copy edited by Gus Mitchell. April 2022
Introduction Genetic lipodystrophies Acquired lipodystrophies Complications Diagnosis Differential diagnoses Treatment
What is lipodystrophy?
Lipodystrophies are conditions that involve the loss of body fat, in particular subcutaneous adipose tissue in the absence of malnutrition or a catabolic state that would otherwise explain the fat loss.
The numerous forms of lipodystrophy feature variable and sometimes distinctive patterns of fat loss. These can be generalised, partial, or localised, and in the majority the fat loss is irreversible. The majority of the lipodystrophies are rare with the exception of HAART-induced, and localised lipodystrophy.
These conditions can be the result of many causes including congenital or acquired, often as a result of autoimmune processes or medications.
Depending on the severity of fat loss, patients can suffer from various metabolic complications with potentially serious health outcomes.
Genetic lipodystrophies
Congenital generalised lipodystrophy
Congenital generalised lipodystrophy (CGL) is a genetic lipodystrophy characterised by a generalised lack of fat, present from birth or developing within the first year of life. This striking loss of fat reveals prominent musculature and veins, and as a result CGL is often diagnosed at birth or in early childhood.
There are several subtypes of CGL, all of which have an autosomal-recessive pattern of inheritance.
Children with CGL exhibit hyperphagia as a result of low serum leptin, a hormone involved in regulating appetite.
Other features include:
- Accelerated growth
- Advanced bone age
- Acanthosis nigricans
- Enlargement of the hands, feet, and jaw suggestive of acromegaly.
Severe metabolic complications are a major feature of CGL, and include:
- Adolescent onset diabetes with high insulin levels due to insulin resistance.
- Severe hypertriglyceridemia resulting in pancreatitis.
- Early enlargement of the liver and spleen can occur as well as severe hepatic steatosis which can progress to cirrhosis and liver failure.
- Females may also suffer from irregular periods, polycystic ovaries, infertility, and hirsutism.
Familial partial lipodystrophy
Familial partial lipodystrophy (FPLD) is a genetic lipodystrophy that usually begins in late childhood or puberty. It is characterised by progressive loss of fat from the upper and lower limbs and gluteal region. There may also be variable fat loss around the trunk. Additionally, patients can accumulate excess fat around the face and neck, giving the appearance of a “buffalo hump” which may raise suspicion of Cushing syndrome.
Fat loss may be subtle and difficult to detect clinically, particularly in males for whom a muscular appearance can be normal.
There are several subtypes of FPLD, most of which have an autosomal-dominant pattern of inheritance.
Other features:
- Severe hypertriglyceridemia is common, resulting in pancreatitis.
- Cardiac conduction system abnormalities, cardiomyopathies, and myopathies may also occur.
- Acanthosis nigricans and hepatic steatosis are less severe in FPLD compared to CGL.
- For women, metabolic complications, features of masculinisation, and irregular periods are more common in those who have excess fat accumulation.
- Despite a high prevalence of polycystic ovarian syndrome, fertility is not commonly affected.
Acquired lipodystrophies
Acquired generalised lipodystrophy
Acquired generalised lipodystrophy (AGL) is characterised by generalised and gradual loss of fat, affecting those born with a normal distribution of fat. Fat is lost at a variable rate ranging from weeks to years and affects all areas of the body, in particular the limbs and face. Fat may be lost from the palms and soles while there is variable loss of intra-abdominal fat; bone marrow stores and fat around the eyes appear to be spared. Fat loss in AGL usually begins in childhood or adolescence, however, in some rare cases it may begin after age 30. Females are affected more often than males with a ratio of 3:1.
As with CGL, patients with AGL often suffer from severe metabolic complications including diabetes mellitus and hypertriglyceridaemia with associated pancreatitis.
There are 3 main classifications of AGL:
● Panniculitis-associated AGL (~25%)
● Autoimmune AGL, associated with juvenile dermatomyositis (~25%)
● Idiopathic AGL has no clear cause (~50%).
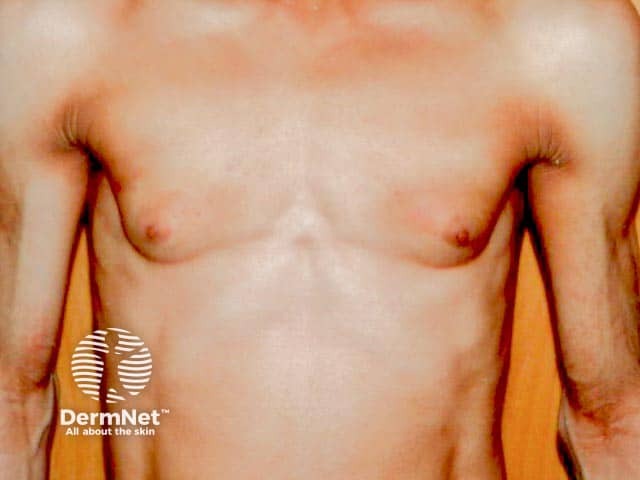
Marked fat loss in a woman over the torso in acquired generalised lipoatrophy

Facial lipoatrophy with peripheral T cell lymphoma

Lipoatrophy in peripheral T cell lymphoma
Acquired partial lipodystrophy
Acquired partial lipodystrophy (APL) is characterised by gradual loss of upper body fat, including the upper trunk, arms, neck, and face, often beginning in late childhood or adolescence. Fat in the lower part of the body including the legs, hips, and lower abdomen tends to be spared, with fat often accumulating in these areas in females post-puberty. Females are affected more often than males with a ratio of 4:1.
Patients are less likely to suffer from metabolic complications compared to other types of lipodystrophy. However, around a fifth of all patients suffer from membranoproliferative glomerulonephritis with some going on to require renal transplantation due to end-stage renal failure.
APL is associated with autoimmune disorders, with the majority of patients having low levels of circulating serum complement 3 and a circulating autoantibody known as complement 3 nephritic factor.

Acquired progressive acral lipoatrophy over the buttock

Acquired progressive acral lipoatrophy (fat loss) on lower arm, preservation over deltoids
Bone marrow transplant-associated lipodystrophy
Bone marrow transplant-associated lipodystrophy is a form of APL affecting patients that have undergone treatment for childhood leukaemia which included total body irradiation, chemotherapy, and allogeneic bone marrow grafting. The pattern of fat loss and associated complications are similar to FPLD.
HAART-induced lipodystrophy
HAART-induced lipodystrophy occurs in HIV patients receiving highly active antiretroviral therapy (HAART) most often after 3-4 years of treatment. HAART-induced lipodystrophy features fat loss from the arms, legs, and face with excess fat accumulation around the neck, upper trunk, and intra-abdominally.
Localised lipodystrophy
Localised lipodystrophy is the most common form of fat loss and can affect single or multiple areas ranging from a small dent in the skin, whole areas of a limb, or large areas of the trunk. Metabolic complications are not a feature of localised lipodystrophy as the degree of fat loss is trivial.
- Drug-induced localised lipodystrophy can occur at the site of injection of medications such as insulin, steroids, and antibiotics.
- Pressure-induced localised lipodystrophy can result from repeated pressure and trauma which often resolves when pressure is avoided.
- Panniculitis-associated localised lipodystrophy is the result of an inflammatory process involving the subcutaneous fat and is associated with autoimmune diseases such as lupus.
- Idiopathic localised lipodystrophy may also occur with no cause identified.
- Centrifugal lipodystrophy is a peculiar variety with no known cause which affects infants, particularly those of Asian descent. There is a pattern of centrifugal fat loss around the abdomen and groin. Often self-resolves in late childhood with no intervention required.

Steroid injection induced lipoatrophy on the arm

Semicircular lipoatrophy over the upper thigh

Idiopathic localised facial lipoatrohpy
What are the complications of lipodystrophy?
Metabolic complications in lipodystrophy can be severe and life-threatening. They are more common in those with a greater extent of fat loss, especially the generalised lipodystrophies. CGL and AGL feature reduced levels of leptin, causing over-feeding which results in the abnormal deposition of fat in other organs with associated metabolic complications, such as:
- High insulin levels resulting in insulin-resistant diabetes
- Hypertriglyceridemia causing recurrent attacks of pancreatitis
- Polycystic ovarian syndrome, infertility, and masculinisation in females
- Fatty liver disease, which can progress to liver cirrhosis and eventual liver failure
- Enlargement of the liver and spleen
- Hypertension and cardiovascular disease.
Other complications include:
- Kidney disease
- Peripheral T-cell cutaneous lymphoma, occuring in 7% of AGL
- Significant psychological distress resulting from the appearance of fat loss
- Physical discomfort arising from the loss of fat pads from the buttocks and feet.
How is lipodystrophy diagnosed?
- History and clinical examination with a focus on onset and pattern of fat loss.
- Assessment of metabolic status and presence of autoimmune diseases.
- Family history, which may include gene testing of the individual and their relatives.
- Low serum leptin is present in generalised lipodystrophies, however, serum leptin levels are not diagnostic.
What is the differential diagnosis for lipodystrophy?
- Uncontrolled diabetes: though with adequate control, fat loss is reversible
- Conditions with severe weight loss including malnutrition, anorexia nervosa, cachexia, HIV, thyrotoxicosis, adrenal insufficiency, and infections
- Cushing syndrome, truncal obesity, and multiple symmetric lipomatosis for FPLD
- Acromegaly for CGL
What is the treatment for lipodystrophy?
Lipodystrophy cannot be cured. Management focuses on reducing the risk of associated metabolic complications and improving cosmetic appearance:
- Energy restricted diets in adults with balanced macronutrients
- Avoidance of overfeeding in children
- Low fat diets in acute pancreatitis
- Exercise is encouraged provided there are no contraindications
- Management of diabetes, dyslipidemia, and hypertension with conventional first-line agents
- For localised lipodystrophies, rotation of injection sites can be useful
- Changing HIV medications can be helpful in HAART-induced lipodystrophy
- Cosmetic procedures such as fat transfer, liposuction, dermal fillers, and breast implants.
Leptin replacement therapy with metreleptin (recombinant human methionyl leptin) reduces hyperphagia and improves metabolic abnormalities in patients with generalised lipodystrophies. There is emerging evidence that leptin replacement therapy also improves metabolic abnormalities in partial lipodystrophies with hypoleptinaemia, however, yields less benefit compared to treatment of generalised lipodystrophies.
Bibliography
- Araújo-Vilar D, Santini F. Diagnosis and treatment of lipodystrophy: a step-by-step approach. J Endocrinol Invest. 2019;42(1):61–73. doi:10.1007/s40618-018-0887-z. Journal
- Brown RJ, Araujo-Vilar D, Cheung PT, et al. The Diagnosis and Management of Lipodystrophy Syndromes: A Multi-Society Practice Guideline. J Clin Endocrinol Metab. 2016;101(12):4500–11. doi:10.1210/jc. 2016–2466. Guideline
- Hussain I, Garg A. Lipodystrophy Syndromes. Endocrinol Metab Clin North Am. 2016;45(4):783-797. doi:10.1016/j.ecl.2016.06.012. Journal
- Melvin A, Stears A, Savage DB. Recent developments in lipodystrophy. Curr Opin Lipidol. 2019;30(4):284–90. doi:10.1097/MOL.0000000000000613. Journal
On DermNet
- Diabetic skin disease
- Deep skin disorders
- Lipodystrophy images
- Panniculitis
- Skin signs of rheumatic disease
Other websites
- Lipodystrophy.info at UT Southwestern
- Berardinelli-Seip Congenital Lipodystrophy — GeneTests GeneReviews
- Lipomatosis and lipodystrophies — Therapeutics in Dermatology
