Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lichen simplex of the scrotum — extra information
Lichen simplex of the scrotum
Authors: Nicole S Kim, Medical Student, University of Toronto, Toronto, Canada; Dr Yuliya Velykoredko, Dermatology Resident, University of Toronto, Toronto, Canada. DermNet Editor in Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. September 2018.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is lichen simplex of the scrotum?
Lichen simplex of the scrotum is a pruritic form of dermatitis in which excessive scratching or rubbing leads to lichenification. Characteristically, there are well-demarcated, erythematous or hyperpigmented plaques with marked skin thickening on one or both sides of the scrotum. Lichen simplex is typically secondary to an underlying skin condition or neuropathy causing extreme itch, such as allergic contact dermatitis.
Lichen simplex is also known as lichen simplex chronicus and neurodermatitis. Lichen simplex of the scrotum is also known as lichen simplex of the male genitalia and 'wash leather scrotum' [1–5].

Lichen simplex of the scrotum
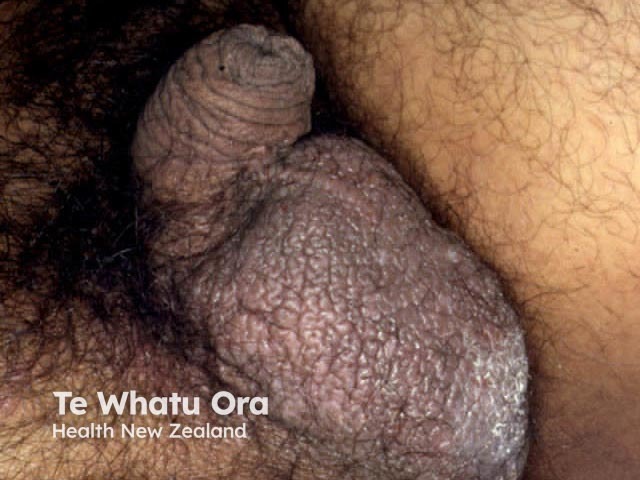
Lichen simplex scrotum

Lichen simplex scrotum
Who gets lichen simplex of the scrotum?
Lichen simplex of the scrotum is most often diagnosed in men between the ages of 35 and 50 years [5].
What causes lichen simplex of the scrotum?
Lichen simplex of the scrotum is attributed to a persistent itch–scratch cycle. Underlying pruritus, a cutaneous or systemic condition, or neuropathy or psychiatric disorder can induce intractable scratching that leads to hypertrophy of the scrotal skin. Contributing factors to scrotal lichen simplex may include [1–3,5]:
- Underlying atopic dermatitis
- Another pruritic skin disorder (eg, psoriasis or lichen planus)
- Contact with an irritant (irritant contact dermatitis) — often triggered by heat, sweating, friction from clothing, or the excessive use of cleansers or topical medicaments
- Contact with an allergen (allergic contact dermatitis)
- Cutaneous infection — usually fungal in origin, generally either candidiasis or a dermatophyte fungus (tinea cruris)
- Psychiatric disorder (eg, anxiety or obsessive-compulsive disorder)
- A benign or malignant skin tumour (eg, squamous cell carcinoma)
- Localised neuropathic itch
- A systemic cause of generalised itch (eg, renal failure, obstructive biliary disease, hyperthyroidism or hypothyroidism, or Hodgkin lymphoma).
What are the clinical features of lichen simplex of the scrotum?
Lichen simplex of the scrotum manifests with clearly demarcated thickening of the scrotal skin with hypopigmentation and hyperpigmentation and variable scale. It is often unilateral, but it may also be bilateral. Coalescing papules form solitary or multiple plaques. Other features may include [3–5]:
- Excoriations and fissures
- Exaggerated skin lines
- Varying degrees of erythema
- A scarcity of hair; or short, broken-off hair shafts.
Signs of an underlying skin disorder may also be noted adjacent to lichen simplex of the scrotum and on another body site.
More areas of lichen simplex may also be found, most commonly on the neck, the scalp, the extensor surfaces of extremities, or the lower legs and ankles [1,2].
What are the complications of lichen simplex of the scrotum?
Complications of lichen simplex of the scrotum may include:
- Insomnia or poor quality of sleep — sleep studies have revealed sleep disturbances due to chronic scratching during sleep
- Secondary bacterial infection (eg, impetigo or cellulitis)
- Post-inflammatory hyperpigmentation or hypopigmentation and, rarely, permanent white marks (leukoderma)
- Fibrosis and scarring from repeated intense scratching
- Structural distortion of the genitals (rarely).
Lichen simplex of the scrotum has also been suspected of contributing to reduced fertility [6].
Adverse effects from treatment can also arise, particularly atrophy due to extended use of a potent topical corticosteroid on the a thin scrotal skin. Topical steroids can also cause pigmentation abnormalities [2,5].
How is lichen simplex of the scrotum diagnosed?
The clinical features of scrotal lichen simplex are generally sufficient to establish the diagnosis. When findings are atypical, further tests can be considered to make a definitive diagnosis or to exclude other similar dermatoses; such tests to be considered include:
- A skin biopsy
- A skin swab for bacteria and candida
- Fungal scraping for dermatophyte fungus
- Patch testing, if allergic contact dermatitis is suspected [3,4].
If the scrotal lichen simplex is associated with generalised pruritus, a workup for systemic causes can be undertaken (as outlined on our pruritus page).
What is the differential diagnosis for lichen simplex of the scrotum?
Other disorders that should be considered in a patient with lichen simplex of the scrotum include [1–3]:
- Lichenified atopic eczema
- Tinea cruris
- Prurigo nodularis
- Psoriasis
- Lichen planus
- Lichen sclerosus
- Mycosis fungoides
- Pemphigoid nodularis
- Condyloma related to human papillomavirus (HPV)
- Skin lesions, tumours, and cancers
- Lumbosacral radiculopathy.
What is the treatment for lichen simplex of the scrotum?
The main goals of treatment for scrotal lichen simplex are:
- Avoiding exacerbating factors
- Breaking the itch–scratch cycle
- Treating any underlying dermatosis or predisposing condition
- Re-establishment of the normal skin barrier.
Short-term topical corticosteroids are used as first-line therapy to break the itch–scratch cycle. Treatment principles for lichen simplex of the scrotum include using a medium potency topical steroid such as triamcinolone ointment until there is a resolution of active lesions. If the disease is refractory after 2–3 weeks of an intermediate-strength corticosteroid, more potent topical steroids can be used on a short-term basis. As the condition improves, the application frequency and potency of the corticosteroid should be decreased to minimise the adverse effects [3,4].
Aim to repair the barrier function of the skin with the frequent application of emollient creams and moisturisers. Minimise environmental triggers such as:
- Dryness
- Sweating or excessive moisture
- Skin friction from tight-fitting or rough materials.
Identify and treat underlying disorders that cause or worsen scrotal lichen simplex [2–5]. Other treatment recommendations include those below.
- Reduce or discontinue using soap, non-prescribed topical medications, and moist wipes.
- Add a barrier cream to protect the skin.
- Treat any underlying inflammatory dermatosis, infection, or systemic cause of the itch.
- Treat psychiatric conditions, such as depression, anxiety, or obsessive-compulsive disorder, with appropriate pharmacotherapy (eg, tricyclic antidepressants or selective serotonin reuptake inhibitors) and psychological therapy.
- Radiculopathy may be managed with tricyclic antidepressants or antiepileptic medications.
What is the outcome for lichen simplex of the scrotum?
The clinical course of scrotal lichen simplex is chronic and protracted, and patients may suffer indefinitely without appropriate treatment. As recurrences occur during psychological stresses or the flare-up of underlying dermatoses, long-term management may be required in some patients [3].
References
- Bolognia JL, Schaffer JV, Cerroni L (eds). Dermatology, 4th edn. Philadelphia: Elsevier, 2018.
- Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K (eds). Fitzpatrick's dermatology in general medicine, 8th edn. New York: McGraw-Hill, 2012.
- Lynch PJ. Lichen simplex chronicus (atopic/neurodermatitis) of the anogenital region. Dermatol Ther 2004; 17(1): 8–19. DOI: 10.1111/j.1396-0296.2004.04002.x. Journal
- Krishnan A, Kar S. Scrotal dermatitis — can we consider it as a separate entity? Oman Med J 2013; 28: 302–5. DOI: 10.5001/omj.2013.91. PubMed Central
- Swick BL. Lichen simplex chronicus. BMJ Best Practice. Lichen simplex chronicus. Updated March 2018. Available at: http://bestpractice.bmj.com/topics/en-gb/625 (accessed 18 September 2018).
- Hendry WF, Munro DD. "Wash leather scrotum" (scrotal dermatitis): a treatable cause of male infertility. Fertil Steril. 1990 Feb; 53: 379–81. PubMed
On DermNet
