Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Hypogonadism in males — extra information
Hypogonadism in males
Author: Dr Gavin Esson, Foundation Trainee, NHS Lothian, Edinburgh, Scotland. DermNet Editor in Chief: Adjunct A/Prof. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. December 2018.
Introduction - hypogonadism Introduction - hypogonadism in males Causes Demographics Clinical features Skin changes Diagnosis Treatment and outcome
What is hypogonadism?
Hypogonadism is the inadequate function of the gonads (reproductive glands) leading to impaired production of germ cells and sex hormones.
What is hypogonadism in males?
Hypogonadism in males refers to diminished testicular function — a reduction in sperm production and in testosterone.
- Primary hypogonadism is due to disease affecting both testes.
- Secondary hypogonadism is due to disease of the hypothalamus or pituitary gland (hypogonadotropic hypogonadism).
What causes hypogonadism in males?
Hypogonadism is due to disruption to any section of the hypothalamic–pituitary–gonadal axis pathway (figure 1).
- The hypothalamus produces gonadotropin-releasing hormone (GnRH).
- GnRH acts on the pituitary gland, which produces follicle-stimulating hormone (FSH) and luteinising hormone (LH).
- FSH stimulates spermatogenesis (development of sperm) in the testes and LH results in the production of testosterone.
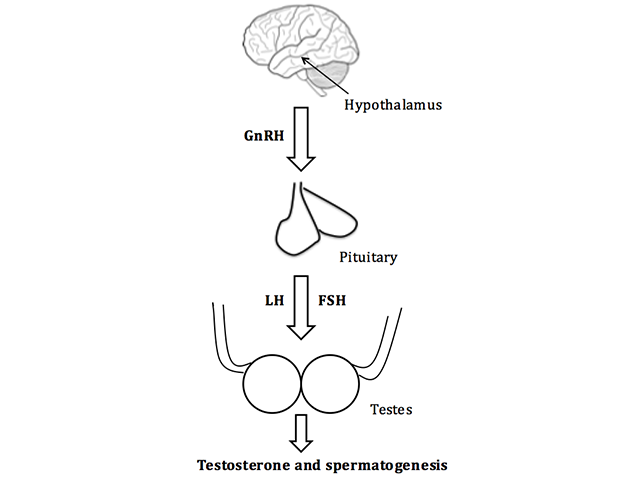
The hypothalamic–pituitary–gonadal axis pathway in males
FSH; follicle-stimulating hormone, GnRH; gonadotropin-releasing hormone, LH; luteinising hormone
Who gets hypogonadism?
Both primary and secondary hypogonadism in males may be congenital or acquired.
Congenital primary hypogonadism
Signs of congenital primary hypogonadism includes:
- Chromosomal abnormalities — the most common being Klinefelter syndrome (XXY karyotype)
- Cryptorchidism
- Myotonic dystrophy (muscle loss) — hypogonadism manifests in adulthood
- Varicocele (swelling of the veins in the scrotum)
- Disorders of androgen synthesis (rare)
Acquired primary hypogonadism
Acquired primary hypogonadism may be result of:
- Infection, especially with mumps orchitis
- Medication — particularly from the use of alkylating agents, suramin, ketoconazole, and glucocorticoids
- Radiation
- Trauma
- Testicular torsion
- Autoimmune polyglandular syndrome type 1
- Chronic systemic disease — liver cirrhosis, chronic kidney disease, and human immunodeficiency virus (HIV) infection
- Idiopathic causes.
Congenital secondary hypogonadism
Congenital secondary hypogonadism results from isolated gonadotropin deficiency due to genetic mutations, such as Kallmann syndrome, Prader–Willi syndrome, and other similar conditions.
Acquired secondary hypogonadism
Acquired secondary hypogonadism may result from:
- Damage to the pituitary or hypothalamus, including:
- Intracranial space-occupying lesions (eg, tumours and cysts)
- Infiltrative disease (eg, sarcoidosis and haemochromatosis)
- Infection (eg, meningitis)
- Pituitary apoplexy (bleeding into pituitary gland)
- Trauma
- Suppression of gonadotropins as a result of:
- Chronic disease (eg, diabetes, anorexia, obesity, and renal disease)
- Critical illness
- Chronic opiate, glucocorticoid, or anabolic steroid use
- Hyperprolactinaemia (an excess of the milk-inducing hormone prolactin).
What are the clinical features of hypogonadism in males?
The clinical features of hypogonadism depend on the patient's age at presentation.
Testosterone deficiency at birth
Hypogonadism at birth may be recognised by ambiguous genitalia (external genitals that are neither clearly male nor clearly female).
Testosterone deficiency pre-puberty
Hypogonadism pre-puberty may be diagnosed by the failure to undergo or complete puberty. The boy may have a young appearance, lack pubic hair, have small genitalia and testes, his voice may fail to break, and he may have difficulty in gaining muscle.
Testosterone deficiency after completion of puberty
After the completion of puberty, the features of hypogonadism include decreased libido, erectile dysfunction, osteoporosis, depression, gynaecomastia, shrinking of the testes, and infertility. After some years of testosterone deficiency, decreased muscle mass and body hair may be evident.
What skin changes may be due to hypogonadism in males?
Androgens are responsible for sebaceous gland growth and differentiation, hair growth, and epidermal barrier homeostasis [1].
Androgen deficiency results in:
- Dry, thin, and wrinkled skin
- Lack of hair growth on the chest, axilla, face, and genitals
- Lack of genital pigmentation
- Gynaecomastia
- Reduced incidence of acne [2,3].
How is hypogonadism in males diagnosed?
The diagnosis of hypogonadism is based on observing typical clinical features in a man with low serum testosterone. The patient should be referred to a specialist.
Initial investigations should include measuring LH, FSH, and serum testosterone (usually taken in the morning, and repeated at least twice). If testosterone is low:
- Elevated LH and FSH suggest primary hypogonadism
- Low LH and FSH suggest secondary hypogonadism.
Further investigations should be directed at identifying the underlying cause.
What is the treatment and outcome for hypogonadism in males?
Effective testosterone replacement in men with hypogonadism has been showed to maintain secondary sexual characteristics, increase libido, muscle strength, fat-free mass, and bone density [4].
Adverse effects of testosterone replacement include:
- Acne
- Prostate enlargement
- Stimulation of the growth of breast cancer or prostate cancer
- Sleep apnoea
- Heart failure
- Erythrocytosis.
What are the contraindications to testosterone therapy?
Testosterone should not be started in individuals with breast cancer, prostate cancer or an increased risk of prostate cancer, haematocrit above 50%, untreated obstructive sleep apnoea, severe lower urinary tract symptoms, or uncontrolled heart failure [4].
References
- Zouboulis CC, Degitz K. Androgen action on human skin — from basic research to clinical significance. Exp Dermatol 2004; 13 Suppl 4: 5–10. PubMed
- Kohn FM, Ring J, Schill WB. [Dermatological aspects of male hypogonadism]. Hautarzt 2000, 51: 223–30. [German] PubMed
- Snyder PJ. Clinical features and diagnosis of male hypogonadism. UpToDate. Available at: www.uptodate.com/contents/clinical-features-and-diagnosis-of-male-hypogonadism (accessed September 2018).
- Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2010; 95: 2536–59. DOI: 10.1210/jc.2009-2354. PubMed
On DermNet
