Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Disseminated superficial actinic porokeratosis — extra information
Disseminated superficial actinic porokeratosis
Author: Dr Amanda Oakley, Dermatologist, New Zealand,1997. Updated 2017; further minor update June 2023
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Sun protection
What is disseminated superficial actinic porokeratosis?
Disseminated superficial actinic porokeratosis, or DSAP, is an inherited keratinisation disorder that causes discrete dry patches on the arms and legs.
DSAP is a special type of inherited 'sunspot". The name porokeratosis means scaly pore and is a misnomer as porokeratosis is not related to pores.





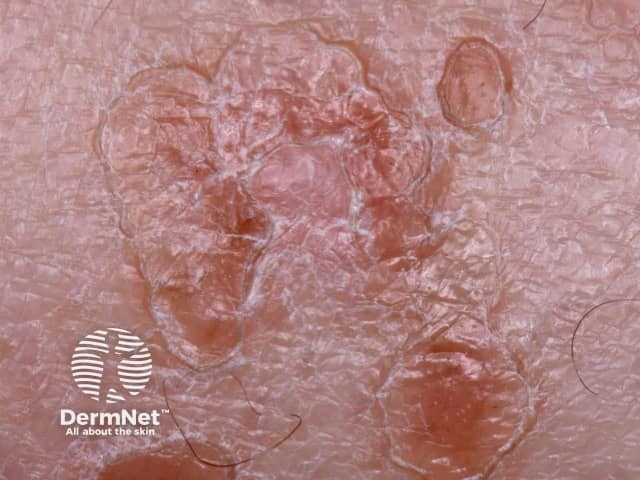
DSAP close-up
Who gets disseminated superficial actinic porokeratosis?
DSAP most often affects people of European descent, although it has also been reported to affect individuals of other races. It is more common in women than in men.
The average age at which patients first notice DSAP is about 35–40 years and its frequency in affected families increases steadily with age. It is rare in childhood.
DSAP may arise in immune-suppressed patients, including after organ transplantation. Its onset can also be triggered by sun exposure, phototherapy, injury, infection or systemic disease.
What causes disseminated superficial actinic porokeratosis?
DSAP is due to a genetic mutation. The tendency to DSAP is inherited as an autosomal dominant characteristic, which means on average half of the children of an affected parent will also have the tendency.
The causative genes in porokeratosis have included the mevalonate pathway genes MVD, MVK, FDPS, PMVK and SART3 genes. These result in decreased cholesterol in the affected areas of the skin.
What are the clinical features of disseminated superficial actinic porokeratosis?
DSAP mainly affects the lower arms and legs bilaterally and arises more frequently on the lower legs. There may be few or innumerable lesions. The forehead and cheeks are affected in less than 10% of individuals and DSAP almost never occurs on the scalp, palms or soles. It tends to be more prominent in the summer and may appear less prominent in winter. New lesions have been provoked by ultraviolet light in sun lamps.
The lesions are composed of multiple irregular roundish, annular or polycyclic plaques, each of which has an elevated horny rim. The visibility of this rim is markedly accentuated by the application of an artificial tanning solution (dihydroxyacetone).
The smallest DSAP lesion is a 1–3 mm conical papule, skin coloured, brownish-red or brown in colour. It is based around a hair follicle containing a keratotic (scaly) plug. Larger plaques have a sharp, slightly raised, keratotic ring, a fraction of a millimetre thick, with a diameter of 10 mm or more. The skin within the ring is thinned and mildly reddened or slightly brown, and a pale ring may be seen just within the ridge. The ridge itself is often a darker brown than the rest of the lesion. The central area is most often pale and smooth, but it may be red, scaly, dry, or have scaly follicular plugs.
Sweating is absent within the lesions. Although most often asymptomatic, sun exposure or heat may cause them to itch or sting.
What are the complications of DSAP?
The development of squamous cell carcinoma (SCC) within a DSAP lesion is the main concern. This is uncommon (< 10% of individuals with DSAP develop SCC). However, many patients with DSAP have had significant exposure to the sun and may also have actinic keratoses and other forms of skin cancer (particularly basal cell carcinoma). SCC presents as a solitary tender enlarging scaly or ulcerated plaque or nodule.
How is DSAP diagnosed?
The diagnosis of porokeratosis is usually clinical, with the help of dermoscopy. DSAP is sometimes diagnosed by finding characteristic features on pathology, in which the scaly rim of DSAP is described as a parakeratotic cornoid lamella. The diagnosis can also be missed on a biopsy if the specimen does not include the rim, it is poorly orientated, or the pathologist's attention is not drawn to the horny ridge seen clinically.
What is the differential diagnosis of DSAP?
There are several kinds of porokeratosis, and these can occur in family members or in the patient that has DSAP.
DSAP is sometimes confused with multiple actinic keratoses, but actinic keratoses are more likely to arise on the face and hands and have a central scale rather than a peripheral scale.
What is the treatment for DSAP?
Compounded off-label topical 2% lovastatin with or without topical cholesterol is the most promising treatment for DSAP so far described.
Over the years the other agents that have been tried include:
- Cryotherapy
- 5-Fluorouracil cream
- Imiquimod cream
- Tretinoin cream
- Ingenol mebutate gel
- Alpha hydroxy acid cream
- Calcipotriol ointment
- Diclofenac gel
- Oral acitretin
- Photodynamic therapy
- Grenz ray therapy
- Laser treatments.
To date, no treatment has proved effective long term. Most people settle for just having the larger lesions frozen lightly and returning as necessary for further treatments, using a moisturiser to reduce the dry feeling.
If the DSAP has been induced by drug-induced immune suppression, withdrawal of the drug has been reported to result in remission of DSAP.
Sun protection
Restriction of sun exposure by wearing long sleeves, skirts or slacks and using sunscreens on the legs and arms is believed to reduce or delay the development of new lesions.
References
- Atzmony L, Lim YH, Hamilton C, Leventhal JS, Wagner A, Paller AS, Choate KA. Topical cholesterol/lovastatin for the treatment of porokeratosis: A pathogenesis-directed therapy. J Am Acad Dermatol. 2020 Jan;82(1):123–31. doi: 10.1016/j.jaad.2019.08.043. Epub 2019 Aug 23. PMID: 31449901; PMCID: PMC7039698.
- Kanitakis J. Porokeratoses: an update of clinical, aetiopathogenic and therapeutic features. Eur J Dermatol. 2014 Sep-Oct;24(5):533–44. doi:10.1684/ejd.2014.2402. Review. PubMed PMID: 25115203. PubMed.
- Liu Y, Wang J, Qin Y, Huang C, Archacki S, Ma J, Li D, Liu M. Identification of three mutations in the MVK gene in six patients associated with disseminated superficial actinic porokeratosis. Clin Chim Acta. 2016 Feb 15;454:124–9. doi: 10.1016/j.cca.2016.01.009. Epub 2016 Jan 12. PubMed PMID: 26794421.
- Santa Lucia G, Snyder A, Lateef A, et al. Safety and Efficacy of Topical Lovastatin Plus Cholesterol Cream vs Topical Lovastatin Cream Alone for the Treatment of Disseminated Superficial Actinic Porokeratosis: A Randomized Clinical Trial. JAMA Dermatol. 2023;159(5):488-495. doi:10.1001/jamadermatol.2023.0205 Journal
- Zhu T, Tian D, Zhang L, Xu X, Xia K, Hu Z, Xiong Z, Tan J. Novel mutations in mevalonate kinase cause disseminated superficial actinic porokeratosis. Br J Dermatol. 2018 Dec 30. doi: 10.1111/bjd.17596. [Epub ahead of print] PubMed PMID: 30597534. PubMed.
On DermNet
- Linear porokeratosis
- Porokeratosis of Mibelli
- Porokeratosis ptychotropica
- Porokeratosis – pathology
- Actinic keratoses
- Basal cell carcinoma
- Squamous cell carcinoma
- Sun protection
- Sunscreens
Other websites
- Porokeratosis — Medscape Reference
- Disseminated superficial actinic porokeratosis — British Association of Dermatologists
- Search for "porokeratosis" on OMIM.org
