Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Costello syndrome — extra information
Costello syndrome
Author: Dr VN Hiromel de Silva, Dermatology Registrar, Waikato Hospital, Hamilton, New Zealand, 2008. Updated by Dr Arun Gangakhedkar, Paediatrician, Waitemata District Board, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. November 2018.
Introduction Causes Clinical features Dermatological manifestations Diagnosis Differential diagnoses Risk of cancer Treatment
What is Costello syndrome?
Costello syndrome is a rare genetic condition in which affected individuals have a distinct facial appearance, curly hair, loose skin, cardiac abnormalities, and cognitive delay.
Costello syndrome is also known as faciocutaneoskeletal syndrome.
What causes Costello syndrome?
Costello syndrome is a RASopathy. it results from a paternal-origin heterozygous germline mutation of the HRAS gene present on chromosome 11p15.5. The mutations are restricted to a narrow spectrum on the p.Gly12Ser residue of HRAS. HRAS normally controls cellular differentiation and function.
- A mutation results in an uncontrolled RAS mitogen-activated protein kinase (MAPK) pathway hyperactivity from a lack of normal suppression by HRAS.
- This leads to the growth of benign and malignant tumours.
- Phenotypic variation may be seen due to other modifying factors.
- Germline mutations are seen in most individuals with Costello syndrome, while somatic mutations with a loss of heterozygosity are associated with malignancies.
Costello syndrome typically results from a de novo mutation so there is no family history of the disorder. Men and women are affected equally [1–8].
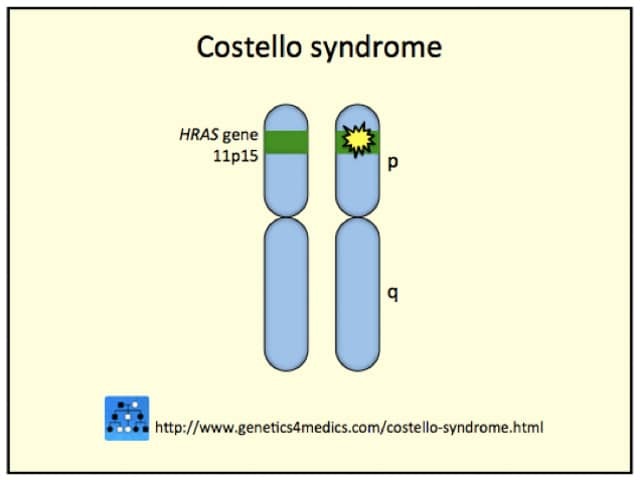
Costello syndrome genetics*
*Credit: Genetics 4 Medics.
What are the clinical features of Costello syndrome?
The symptoms of Costello syndrome evolve over a period of time and developmental delay is common. The key clinical features are:
- Macrocephaly (large head) and macrosomia (large body) at birth
- Coarse facial features
- Hypoglycaemia (low blood sugar)
- Feeding difficulties and postnatal growth retardation
- Unexplained tachyarrhythmia (elevated heart rate)
- Hypotonia (low muscle tone)
- Hoarse voice.
Perinatal features may include:
- Premature delivery
- Excessive amniotic fluid in the womb (leading to conditions such as hydrops and polyhydramnios)
- Macrosomia with nuchal thickening
- Short long bones and abnormal hand posture
- Cardiac and renal anomalies on an antenatal scan
- Fetal tachyarrhythmia
- Lymphatic dysplasia.
Hyperpigmentation of skin with deep creases and loose skin on the hands and feet should raise the clinical suspicion of Costello syndrome during infancy. Other features that can occur throughout the patient's life can include:
- Characteristic facial features:
- Macrocephaly with a high forehead
- Bitemporal narrowing
- Large-cupped and posteriorly rotated ears with folded earlobes
- A flat nasal bridge with epicanthic folds
- A square mandible with a pointed chin
- A prominent tongue
- Full cheeks and lips with a wide mouth
- Characteristic features of the hands:
- Hypermobile with ulnar deviation
- Splayed fingers with spatulate tips
- Orthopaedic problems:
- A short neck and inverted neck curve (cervical kyphosis)
- Spinal abnormalities
- Chest deformity with sternum and rib-cage asymmetry
- Joint laxity with positional foot deformity
- Tight Achilles tendon.
- Characteristic skin, hair, and nail changes (detailed below)
- Short stature
- Relative macrocephaly
- Difficulty with eating
- Developmental disabilities [1–9].

Costello syndrome
What are the dermatological manifestations of Costello syndrome?
Ectodermal defects involving skin, hair, nails, and mucosal changes are common and often distinguishing.
Skin
The main dermatological manifestations of Costello syndrome can include:
- Velvety soft and redundant skin on the neck, hands, and feet
- Hyperkeratosis of the palms and soles, and calluses over dorsal aspects of the hands and feet
- Loose skin with deep palmar and plantar creases
- Distal fingertip creases with pachydermatoglyphia and stippled dermatoglyphics (fingerprints) evolving with age
- Pachydermatoglyphia, seen clinically as an exaggerated pattern of ridges on the palms and fingertips and histologically as marked epidermal hyperkeratosis, acanthosis, papillomatosis, and hypergranulosis
- Periorificial papillomas in perinasal, perioral and perianal areas; these may also be seen on the torso, extremities, and axillae; papillomas appearing as skin tags or sessile nodules may also be viral warts or keratoses and these typically manifest after infancy
- Pachydermatoglyphia, malignant acanthosis nigricans, and florid cutaneous papillomatosis occurring in the same patient may suggest a dysregulation of transforming growth factor‐alpha or epidermal growth factor.
Nails
Nail defects in Costello syndrome manifest as slow-growing, triangular, and brittle dystrophic fingernails with longitudinal striations.
Hair
Changes to the hair in Costello syndrome can include:
- Hair that may be blonde or pigmented, but different in type from that of other family members
- Thin and kinky hair with tight curls that give a frizzy ‘cloud of curls’ appearance
- Thick eyebrows and unusually long eyelashes — sometimes requiring a regular trim.
Alopecia may be seen but this is a more common feature in cardiofaciocutaneous syndrome. Hair loss with skin changes gives a prematurely aged appearance in adults.
Pigmentation abnormalities
Generalised hyperpigmentation of skin is seen in a third of individuals; acanthosis nigricans is also reported in a third of the affected population with velvety plaques occuring on the neck and flexural areas, and sometimes on the posterior earlobes — these can be verrucous in older individuals.
Mucosa
An oral examination for gingival hypertrophy and mucocutaneous lip papules is important, as these are both distinct features of Costello syndrome.
Photosensitivity
Over half of individuals with Costello syndrome do not like sun exposure or are extremely photosensitive, and three-quarters of affected individuals report heat intolerance.
How is Costello syndrome diagnosed?
Prenatal diagnosis is suspected from the phenotypic features, and antenatal confirmative HRAS mutation testing has been reported.
Postnatal diagnosis is confirmed by identifying the HRAS mutations. Over 80% of affected individuals have mutations affecting the p.Gly12Ser residue and, less commonly, p.Gly12A. Rare mutations associated with either a mild or severe phenotype have been described.
Routine chromosomal microarray and karyotype testing may be non-diagnostic [1–13].
What is the differential diagnosis for Costello syndrome?
Overgrowth syndromes, such as Beckwith–Wiedemann syndrome and Simpson–Golabi–Behmel syndrome, with macrosomia and hypoglycaemia may be confused with Costello syndrome in the neonatal period.
Congenital myopathy syndromes with hypotonia may also be mistaken for Costello syndrome.
- Cutis laxa syndrome due to an underlying elastin deficiency results in pendulous skin folds and a characteristic ‘bloodhound’ facial appearance as if the skin is too large for the body.
- Mucopolysaccharidoses syndromes (a metabolic disease due to an absence of sugar-digesting enzymes) may present with coarse facial features, hair changes, organomegaly, and more severe developmental delays.
Like Costello syndrome, other RASopathy syndromes, such as Noonan syndrome, cardiofaciocutaneous syndrome, and Noonan syndrome-like disorder with loose anagen hair syndrome, may also manifest with neonatal macrosomia, coarse facial features, pigmented skin changes, hair abnormalities, failure to thrive, and developmental delay.
- The characteristic facies, skin changes, hand abnormalities, tachyarrhythmias, and feeding difficulties with postnatal growth retardation help differentiate Costello syndrome from other macrosomia syndromes.
- A chaotic atrial tachyarrhythmia, hypertrophic cardiomyopathy, papillomatosis and hyperkeratosis, and fuller eyebrows and curly hair are more common in Costello syndrome than in Noonan syndrome cardio-facio-cutaneous syndrome.
- Pulmonic stenosis is more common in Noonan syndrome.
- Generalised hyperpigmentation, ulerythema ophryogenes, keratosis pilaris, multiple melanocytic naevi, and vascular malformations are more common in cardio-facio-cutaneous syndrome and Noonan syndrome.
- While there is significant phenotypic overlap among the RASopathy syndromes, individuals with Costello syndrome are more likely to present with cutaneous papillomas, palmoplantar keratoderma and full eyebrows, and are less likely to present with ulerythema ophryogenes, keratosis pilaris or multiple melanocytic naevi [9–13].
What is the risk of cancer in Costello syndrome?
Some somatic mutations in the HRAS gene predispose individuals with Costello syndrome to an increased risk of neoplasms, with a 15% lifetime risk of developing malignant tumours. There is a high risk of developing rhabdomyosarcoma (cancer in the muscles attached to the bones), neuroblastoma (cancer of the nerve tissues), or transitional cell carcinoma of the bladder during childhood and adolescence [1–13].
What is the treatment for Costello syndrome?
There is no cure for Costello syndrome. However, there are recommended general supportive measures for managing the syndrome. These include:
- A multidisciplinary team approach
- Parental education and support
- Enteral nutrition with nasogastric or gastric tubes during infancy
- Physical therapy for musculoskeletal complications
- Physiotherapy, occupational therapy, speech and language therapy, and developmental therapy support, including the use of assistive technology
- Airway and breathing interventions if there are any anatomical abnormalities
- Growth hormone therapy for poor growth and metabolic control
- Orthopaedic interventions as indicated
- Surgery for the neoplastic complications
- Skin lesion treatment with keratolytics (eg, urea cream) for hyperkeratosis, cryotherapy, or the excision of papillomas.
Surveillance and routine skin care should be undertaken to ensure timely recognition, diagnostic evaluation, and prompt therapy.
- Echocardiography for heart arrhythmias
- Abdominal and pelvic ultrasound
- Urine analysis for blood traces
- Tumour surveillance.
Genetic counselling should be offered to all the families with affected children so that they may understand the risk of Costello syndrome in future pregnancies. The risks of neoplasms and the need for surveillance should be discussed. Affected individuals do not go on to have children, but there would be a 50% chance of having affected progeny if they were to reproduce [1–13].
References
- Myers A, Bernstein JA, Brennan ML, Curry C, Esplin ED, Fisher J, et al. Perinatal features of the RASopathies: Noonan syndrome, cardiofaciocutaneous syndrome and Costello syndrome. Am J Med Genet A 2014; 164A: 2814–21. DOI: 10.1002/ajmg.a.36737. PubMed
- Kuniba H et al. Prenatal diagnosis of Costello syndrome using 3D ultrasonography amniocentesis confirmation of the rare HRAS mutation G12D. Am J Med Genet Part A 2009; 149A: 785–7. PubMed
- Henekam RCM. Costello syndrome: an overview. Am J Med Gen Part C 2003; 117C: 42–48. PubMed
- Gripp KW et al. Phenotypic analysis of individuals With Costello syndrome due to HRAS p.G13C. Am J Med Gen Part A 2010: 155:706–716. PubMed
- Digilio MC et al. Costello syndrome: clinical diagnosis in the first year of life. Eur J Pediatr 2008; 167: 621–628. PubMed
- Lione C et al. Understanding growth failure in Costello syndrome: increased resting energy expenditure. J Pediatr 2016; 170: 322–24. PubMed
- Triantafyllou P et al. Growth hormone replacement therapy in Costello syndrome. Growth Horm IGF Res. 2014: 24; 271–275. PubMed
- Kerr B, Grip KW, Lin AE. Costello syndrome in Management of genetic syndromes. Ed Cassidy and Judith E Allanson. John Wiley 2010: 211–25
- Detweiler S et al. Orthopedic manifestations and implications for individuals with Costello syndrome. Am J Med Genet A 2013: 161A; 1940–49. PubMed
- Siegel DH et al. Dermatological phenotype and Ras dysregulation in Costello syndrome: consequences of Ras dysregulation in development. BJD 2012; 166: 601–607. PubMed
- Bertola D et al. Phenotypic spectrum of Costello syndrome individuals harboring the rare HRAS mutation p.Gly13Asp. Am J Med Genet A. 2017; 173: 1309–18. PubMed
- Ngyun V et al. Cutaneous manifestations of Costello syndrome. Int J Dermatol 2007: 46; 72–76. PubMed
- Morice–Picard F et al. Cutaneous manifestations in Costello and cardiofaciocutaneous syndrome: report of 18 cases and literature review. Peditr Dermatol 2013; 30(6): 665–73. PubMed
On DermNet
Other websites
- Costello syndrome US National Library of Medicine Genetics Home Reference
- Costello Syndrome Support Group
- Costello syndrome – OMIM
- International Costello Syndrome Support Group
- The Costello Syndrome Family Network
- Costello Kids
- Costello.CFC (Associazione Italiana sindrome di Costello)
- RASopathies.net
