Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Chronic inducible urticaria — extra information
Chronic inducible urticaria
Author: Donna Bartlett, Medical Writer, Allori, Melbourne, Victoria, Australia. Adjunct A/Prof Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. December 2018.
This article was supported by an educational grant from Novartis, distributors of Xolair™ in New Zealand and Australia. Xolair is not indicated for the treatment of chronic inducible urticaria in either country. Sponsorship does not influence content.
Introduction - urticaria
Introduction - chronic urticaria
Introduction
Demographics
Clinical features
Causes
Complications
Diagnosis
Differential diagnoses
Treatment
Pharmacological treatment
Outcome
What is urticaria?
Urticaria is a condition characterised by the presence of weals (hives) or angioedema (swelling in the skin).
- A weal is a superficial red or pale swelling in the skin that is often surrounded by erythema. A weal can persist from a few minutes to 24 hours.
- Angioedema is a deeper skin-coloured or red swelling within the skin or mucous membranes. It can take up to 72 hours to resolve.
Urticaria affects up to one in four people at some time in their lives and is classified by duration, acute or chronic, and cause, whether spontaneous or inducible.
Acute urticaria is the daily or episodic occurrence of weals, angioedema, or both for less than 6 weeks. Causes can include infections and allergies, but more often, the cause is unknown.
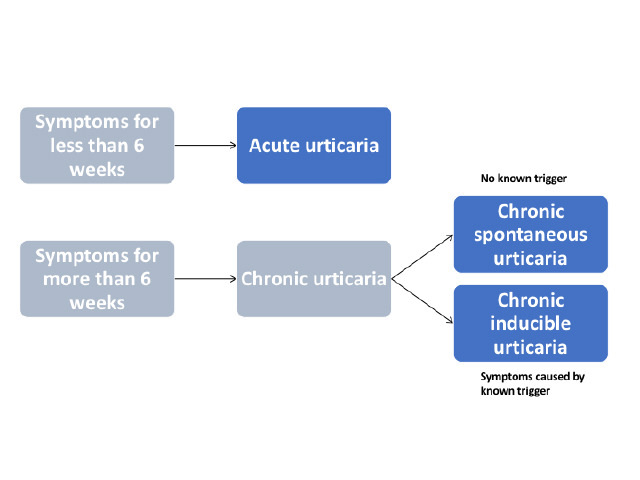
Figure 1 - Classification of urticaria

Spontaneous urticaria

Angioedema

Dermographism
What is chronic urticaria?
Chronic urticaria is the daily or episodic occurrence of weals, angioedema, or both for 6 weeks or more. Chronic urticaria can persist for a duration ranging from a few months to many years.
International guidelines have recently been published for the classification, diagnosis, and management of chronic urticaria, based on a consensus from multiple national and international societies.
Chronic urticaria is either spontaneous or inducible; both types may co-exist in one patient. (See DermNet's page on Chronic spontaneous urticaria).
What is chronic inducible urticaria?
Chronic inducible urticaria is chronic urticaria that has an attributable cause or trigger and is classified according to the stimulus that provokes weals to develop. Commonly, these stimuli that provoke weals to develop include stroking or scratching the skin (dermographism), exercise, and emotional upset (cholinergic urticaria).
Less common forms of chronic inducible urticaria are triggered by cold, heat, pressure, sunlight (solar urticaria), contact with water or various chemicals (contact urticaria), or vibration.
Who gets chronic inducible urticaria?
Chronic urticaria is reported to affect 1.8% of the population. The prevalence of chronic inducible urticaria is approximately 0.5% (15–25% of all cases of chronic urticaria).
Women experience urticaria and chronic urticaria almost twice as often as men. Although urticaria in children is common, they are more likely to present with chronic spontaneous urticaria than with chronic inducible urticaria.
What are the clinical features of chronic inducible urticaria?
Chronic inducible urticaria usually presents with weals. Weals can appear on any site of the body.
- Weals range in size from a few millimetres to several centimetres.
- They are white or red and are often surrounded by a red flare.
- In chronic inducible urticaria, weals generally appear about 5 minutes after the stimulus and last from a few minutes up to 2 hours.
- The weals may change shape before resolving — they may be round, and form rings or a map-like pattern.
Characteristically, weals are:
- Linear in symptomatic dermographism
- Confined to contact areas in contact urticaria
- Confined to contact areas in vibratory urticaria
- Diffuse in cold urticaria (if large areas of skin are affected, angioedema can also occur in cold urticaria).
Vibratory angioedema can very rarely be induced within a few minutes of exposure to a vibratory stimulus. Delayed pressure can lead to urticaria and angioedema.
Symptoms are usually confined to skin areas that are exposed to a specific trigger. Individual patients may exhibit two or more subtypes of chronic inducible urticaria.

Linear weals in dermographism

Round and linear weals in dermographism

Diffuse weal from ice cube test in cold urticaria
What causes chronic inducible urticaria?
Urticaria is a mast cell-driven disease. Activated mast cells release histamine along with other mediators, such as platelet-activating factor and cytokines, resulting in sensory nerve activation, vasodilation, plasma extravasation, and recruitment of cells to the urticarial lesion. Mast cells can be activated by many different molecules in urticaria, but generally, these are not well defined.
Weals and angioedema are induced by environmental or physical stimuli in chronic inducible urticaria. Different types of inducible urticaria and their triggers include:
- Dermographism — triggered by scratching or tight clothing
- Cold urticaria — triggered by cold air, cold water, ice, or cryotherapy
- Cholinergic urticaria — resulting from increased body heat due to exercise, emotional upset, or a hot shower
- Contact urticaria — where a trigger substance is absorbed through the skin or a mucous membrane; this can be an allergen such as latex or semen (immunoglobulin E [IgE] mediated), a pseudo-allergen, or an irritant (such as a medicine, stinging nettle, or a hairy caterpillar)
- Delayed pressure urticaria — resulting from pressure on the affected area several hours earlier, such as from a heavy bag, a seat belt, or sitting on a horse
- Solar urticaria — from exposure to sunlight, mainly affecting skin that is infrequently exposed to the sun
- Heat urticaria — triggered by a hot water bottle or a hot drink
- Aquagenic urticaria or angioedema — triggered by water
- Vibratory angioedema — resulting from vibratory activities such as using a jackhammer, lawn mowing, or motorcycle riding.
What are the complications of chronic urticaria?
The burden of chronic urticaria is substantial for patients, their families and carers, the healthcare system, and society. Chronic urticaria can result in sleep deprivation, anxiety, depression, lack of energy, and social isolation and result in a significant deterioration in the quality of life.
How is chronic inducible urticaria diagnosed?
Chronic inducible urticaria is diagnosed through the taking of a careful history and examination; this diagnosis is based on a history of daily or episodic weals for more than 6 weeks that have been induced by an external stimulus.
International guidelines provide a diagnostic algorithm for chronic urticaria (see figure 2). The diagnosis of chronic inducible urticaria relies on provocation testing and then compiling a thorough history covering:
- When the urticaria began
- The shape, size, frequency, and distribution of the weals
- The presence of angioedema
- The presence of bone or joint pain, fever, or abdominal pain
- A prior or family history of weals and angioedema
- Whether the weals were induced by physical agents or exercise
- Whether the presence of corresponds with a time of day, work, recreation, menstrual cycle, holidays, or travel overseas
- The effect of food or drugs on the urticaria (eg, non-steroidal anti-inflammatory drugs [NSAIDs], and angiotensin-converting enzyme [ACE] inhibitors)
- Any association with infections or psychosocial stress
- Any history of allergies or systemic illness
- Occupational history, hobbies, and activities
- Previous treatment and response
- Diagnostic procedures and results.
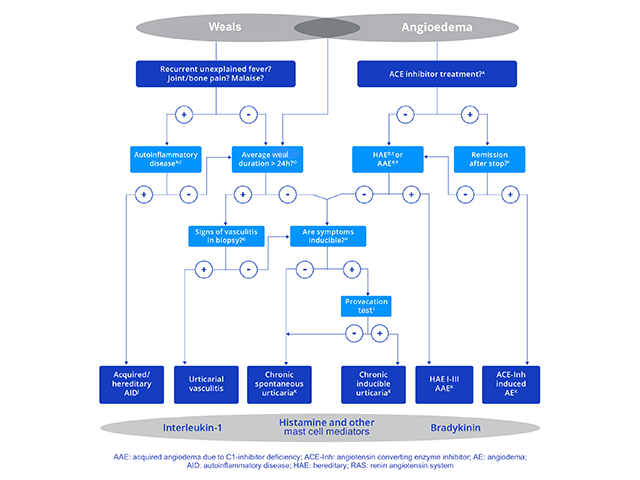
Figure 2 - Diagnostic algorithm for chronic urticaria
Credit: Zuberbier et al, Allergy 2018.
Notes on diagnostic algorithm for chronic urticaria
- Apart from ACE inhibitors, other renin inhibitors and sartans have also been reported to induce angioedema but much less frequently.
- Patients should be asked for detailed family history and age at onset of disease.
- Test for elevated inflammation markers (eg, CRP and ESR), test for paraproteinemia in adults, look for signs of neutrophil-rich infiltrates in skin biopsies, and perform gene mutation analysis for hereditary periodic fever syndromes (eg, cryopyrin-associated periodic syndromes) if strongly suspected.
- Patients should be asked, “How long does each weal last?”
- Test for complement C4, and C1-inhibitor levels and function; also test for C1q and C1-inhibitor antibodies if acquired and angioedema is suspected; and do gene mutation analysis if the former tests are unremarkable but the patient’s history suggests hereditary angioedema.
- If there is no remission after 6 months of ACE-inhibitor discontinuation, test C1-inhibitor levels.
- Does the biopsy of lesional skin show damage to the small vessels in the papillary and reticular dermis and fibrinoid deposits in perivascular and interstitial locations suggestive of urticarial vasculitis?
- Patients should be asked, “Can you make your weals appear? Can you bring out your weals?”
- In patients with a history suggestive of inducible urticaria, standardized provocation testing according to international consensus recommendation should be performed [16].
- Acquired autoinflammatory syndromes include Schnitzler syndrome, systemic juvenile idiopathic arthritis, and adult-onset Stills disease; hereditary autoinflammatory syndrome include cryopyrin-associated periodic syndromes, such as familial cold autoinflammatory syndrome, Muckle-Wells syndrome, and neonatal-onset multisystem inflammatory disease, more rarely hyper-IgD syndrome and tumour necrosis factor receptor associated periodic syndrome.
- In some rare cases, recurrent angioedema is neither mast cell mediator-mediated nor bradykinin-mediated, and the underlying pathomechanisms remain unknown. These rare cases are referred to as ‘idiopathic angioedema’ by some authors.
The consensus recommendations for diagnostic testing and management of chronic inducible urticaria can be used to identify the subtype of chronic inducible urticaria and to assess disease activity.
Provocation testing is used to determine the relevant triggers and to assess trigger thresholds. Provocation testing in positive patients usually results in the development of urticaria within a few minutes. One exception is delayed pressure urticaria, where it may be necessary to wait several hours for a response.
In patients with negative provocation responses, where chronic inducible urticaria is strongly suspected from the patient’s history, the test should be repeated. Ideally, the test should be conducted on a skin site that has previously been affected, although testing should not be done if weals have occurred in this site within the previous 3 days.
The results of provocation tests can be affected by medication; therefore, symptomatic treatment should be ceased before testing if possible. Antihistamines should be stopped 3 days before testing, and systemic glucocorticoids 7 days before testing.
A sample form for the documentation of provocation testing is shown in figure 3.
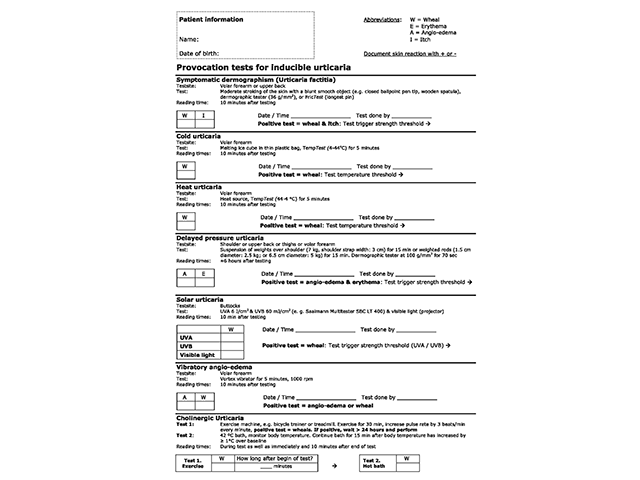
Figure 3 - Provocation tests for inducible urticaria
Credit: Magerl M, et al. Allergy 2016.
What is the differential diagnosis for chronic inducible urticaria?
The differential diagnosis depends on the specific type of chronic inducible urticaria and includes other forms of inducible and spontaneous urticaria, which may co-exist.
- Dermographism and delayed pressure urticaria can present with a similar history.
- Cholinergic urticaria can be confused with exercise-induced anaphylaxis.
- Aquagenic urticaria can be confused with aquagenic pruritus, cholinergic urticaria, cold urticaria, and local heat urticaria.
- Solar urticaria can be mistaken for sunburn or another form of photosensitivity, such as:
Assessment of disease activity and control
In addition to diagnosis, trigger threshold measurements are also used during treatment to measure ongoing disease activity and response to treatment.
The Urticaria Control Test (UCT) is useful in the assessment of patients’ disease status and is validated to determine the level of disease control in both chronic spontaneous urticaria and chronic inducible urticaria. The UCT has only four items with a clear cut-off for ‘well controlled’ versus ‘poorly controlled’ disease, making it useful in routine clinical practice.
The Angioedema Activity Score (AAS) allows the patient to score each of five key factors relating to their symptoms from 0 to 3 (giving a daily score of 0–15). Daily AAS can be summed to provide 7-day (AAS7), 4-week (AAS28), and 12-week (AAS84) scores.
Quality of life
Validated instruments can be used to assess the emotional impact of chronic urticaria and the effect on the patient’s quality of life, such as the Chronic Urticaria Quality of Life Questionnaire (CU-Q2oL) and the Angioedema Quality of Life Questionnaire (AE-QoL).
What is the treatment for chronic inducible urticaria?
Treatment aims to control symptoms.
The approach to the management of chronic inducible urticaria can involve:
- Avoidance of trigger factors
- Induction of tolerance
- Pharmacological treatment to prevent mast cell mediator release or to prevent the effects of mast cell mediators.
Avoidance of trigger factors
It is often difficult for patients with chronic inducible urticaria to completely avoid the physical stimuli that trigger wealing. It is recommended that patients minimise exposure to triggers as much as possible, although the induction of tolerance (described below) requires daily exposure to a trigger.
Inducing tolerance
Inducing tolerance can be useful in cold urticaria, cholinergic urticaria, and solar urticaria. Tolerance induction lasts only a few days, and consistent daily exposure is required to maintain tolerance.
Pharmacological treatment of chronic urticaria
An algorithm to treat chronic urticaria is included in the international guidelines (see figure 4), these guidelines should be used with caution in children and pregnant/lactating women. Drugs that are contraindicated in pregnancy should not be used.
Treatment should be continued as required until the urticaria has cleared up.
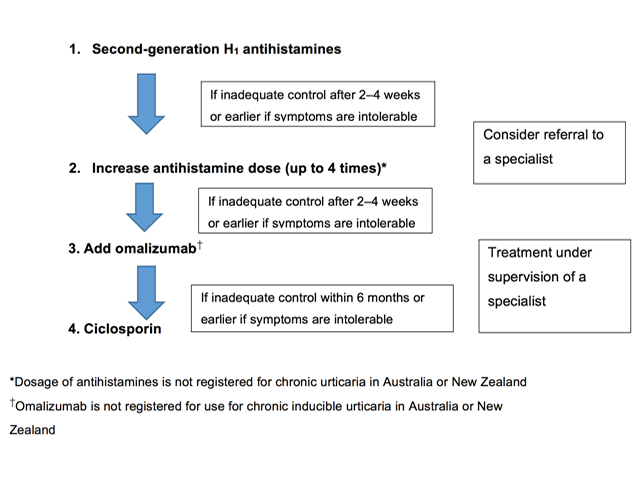
Figure 4 - Pharmacological treatment algorithm for chronic urticaria
Credit: Zuberbier et al, Allergy 2018.
Antihistamines
Some forms of chronic inducible urticaria are mediated by histamine. Intermittent or continuous treatment with H1-antihistamines is supported by clinical trial data.
Non-sedating antihistamines are preferred to older antihistamines, which have anticholinergic effects and sedative actions. First-line symptomatic treatment for chronic inducible urticaria includes:
- Cetirizine
- Ebastine
- Loratadine
- Fexofenadine
- Desloratadine
- Levocetirizine
- Rupatadine
- Bilastine.
Terfenadine and astemizole are no longer available in New Zealand or Australia because they are cardiotoxic in combination with ketoconazole or erythromycin.
If standard doses are not effective, the doses of bilastine, loratadine, cetirizine, desloratadine, ebastine, fexofenadine, levocetirizine and rupatadine can be increased up to four-fold (note that some of these agents are not available and the higher doses are not licensed in New Zealand or Australia).
Most patients with chronic inducible urticaria who do not respond to standard doses of antihistamines will benefit from up-dosing, but antihistamines are not always effective. Localised heat urticaria, aquagenic urticaria, and vibratory urticaria rarely respond to antihistamines.
Treatment of refractory chronic inducible urticaria
About one-third of patients continue to have symptoms despite maximal tolerated daily doses of antihistamine. Patients with refractory chronic inducible urticaria should be referred to a dermatologist, immunologist, or medical allergy specialist.
Omalizumab
Omalizumab has been reported to be effective in chronic inducible urticaria, including cholinergic urticaria, cold urticaria, solar urticaria, heat urticaria, symptomatic dermographism, and delayed pressure urticaria.
Note: Omalizumab is not indicated for the treatment of patients with chronic inducible urticaria in New Zealand or Australia.
Ciclosporin
No published trials have specifically investigated the use of ciclosporin in patients with chronic inducible urticaria, although a case-series (n=100) investigating its use in the management of chronic spontaneous urticaria included patients that also had chronic inducible urticaria (45% of cases). Control was achieved with ciclosporin or omalizumab in some cases refractory to antihistamines.
Note: Ciclosporin is not indicated for the treatment of patients with chronic inducible urticaria in New Zealand or Australia.
Corticosteroids
- Systemic corticosteroids have not been studied in randomised controlled trials, and evidence for their use in chronic inducible urticaria is limited.
- Long-term use of systemic corticosteroids should be avoided as high doses are often required to reduce the symptoms of urticaria with associated potentially serious adverse effects.
- A short course of corticosteroids may be considered in cases of severe exacerbations of chronic inducible urticaria, but this is not always effective.
Phototherapy
Phototherapy has been successful in the treatment of patients with chronic inducible urticaria, particularly in patients with dermographism. The most common form of phototherapy used is narrowband ultraviolet B phototherapy.
Other treatments
There is little evidence to support any other treatments for chronic inducible urticaria.
Immunomodulatory treatments may be of value to individual patients in particular clinical situations (eg, dapsone for cold urticaria).
What is the outcome for chronic inducible urticaria?
Chronic inducible urticaria may resolve with treatment of symptoms and avoidance of physical stimuli that trigger the urticaria. However, in many patients, the threshold for the relevant physical trigger is low and total avoidance of symptoms is almost impossible.
References
- Zuberbier T, Aberer W, Asero R, et al. The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. The 2017 Revision and Update. Allergy 2018; 73: 1392–1414. DOI: 10.1111/all.13397. PubMed
- CSU Working Party, Australian Society of Clinical Immunology and Allergy (ASCIA). Chronic spontaneous urticaria (CSU) guideline. 2020. Available at: https://www.allergy.org.au/images/stories/pospapers/ASCIA_HP_Position_Paper_CSU_2020.pdf [accessed 9 September 2024].
- Borlu M, Levent Cinar S, Kartal D. Chronic inducible urticaria part I. Kartal SP, Kutlubay K (eds). A comprehensive review of urticaria and angioedema. London: IntechOpen, 2017. Available at: https://www.researchgate.net/publication/317323701_Chronic_Inducible_Urticaria_Part_I. (accessed 10 December 2018).
- Maurer M, Weller K, Bindslev-Jensen C, et al. Unmet clinical needs in chronic spontaneous urticaria. A GA2LEN task force report. Allergy 2011; 66: 317–30. DOI: 10.1111/j.1398-9995.2010.02496.x. PubMed
- Kaplan AP. Chronic urticaria and angioedema. N Engl J Med 2002; 346: 175–9. DOI: 10.1056/NEJMcp011186. Journal
- Magerl M, Altrichter S, Borzova E, et al. The definition, diagnostic testing, and management of chronic inducible urticarias — the EAACI/GA2LEN/EDF/UNEV consensus recommendations 2016 update and revision. Allergy 2016; 71: 780–802. DOI: 10.1111/all.12884. PubMed
- Maurer M, Abuzakouk M, Bérard F, et al. The burden of chronic spontaneous urticaria is substantial: real-world evidence from ASSURE-CSU. Allergy 2017; 72: 2005–16. DOI: 10.1111/all.13209. PubMed
- Dice JP, Gonzalez-Reyes. Physical (inducible) forms of urticaria. UpToDate. Updated 4 May 2018. Available at: www.uptodate.com/contents/physical-inducible-forms-of-urticaria (accessed 26 November 2018).
- Weller K, Groffik A, Church MK, et al. Development and validation of the Urticaria Control Test: a patient-reported outcome instrument for assessing urticaria control. J Allergy Clin Immunol 2014; 133: 1365–72.e6. DOI: 10.1016/j.jaci.2013.12.1076. PubMed
- Weller KG, Magerl M, Tohme M, et al. Development, validation and initial results of the Angioedema Activity Score. Allergy 2013; 68: 1185–92. DOI: 10.1111/all.12209. PubMed
- Baiardini I, Pasquali M, Braido F, et al. A new tool to evaluate the impact of chronic urticaria on quality of life: Chronic Urticaria Quality of Life Questionnaire (CU-Q2oL). Allergy 2005; 60: 1073–8. DOI: 10.1111/j.1398-9995.2005.00833.x. PubMed
- Weller K, Groffik A, Magerl M, et al. Development and construct validation of the angioedema quality of life questionnaire. Allergy 2012; 67: 1289–98. DOI: 10.1111/all.12007. PubMed
- Metz M, Bergmann P, Zuberbier T, Maurer M. Successful treatment of cholinergic urticaria with anti-immunoglobulin E therapy. Allergy 2008; 63: 247–9. DOI: 10.1111/j.1398-9995.2007.01591.x. PubMed
- Metz M, Schutz A, Weller K, et al. Omalizumab is effective in cold urticaria-results of a randomized placebo-controlled trial. J Allergy Clin Immunol 2017; 140: 864–7.e5. DOI: 10.1016/j.jaci.2017.01.043. Journal
- Boyce JA. Successful treatment of cold-induced urticaria/anaphylaxis with anti-IgE. J Allergy Clin Immunol 2006; 117: 1415–8. DOI: 10.1016/j.jaci.2006.04.003. PubMed
- Guzelbey O, Ardelean E, Magerl M, Zuberbier T, Maurer M, Metz M. Successful treatment of solar urticaria with anti-immunoglobulin E therapy. Allergy 2008; 63: 1563–5. DOI: 10.1111/j.1398-9995.2008.01879.x. PubMed
- Bullerkotte U, Wieczorek D, Kapp A, Wedi B. Effective treatment of refractory severe heat urticaria with omalizumab. Allergy 2010; 65: 931–2. DOI: 10.1111/j.1398-9995.2009.02268.x. PubMed
- Maurer M, Schutz A, Weller K, et al. Omalizumab is effective in symptomatic dermographism-results of a randomized placebo-controlled trial. J Allergy Clin Immunol 2017; 140; 3: 870–3.e5. DOI: 10.1016/j.jaci.2017.01.042. Journal
- Krause K, Ardelean E, Kessler B, et al. Antihistamine-resistant urticaria factitia successfully treated with anti-immunoglobulin E therapy. Allergy 2010; 65: 1494–5. DOI: 10.1111/j.1398-9995.2010.02409.x. PubMed
- Bindslev-Jensen C, Skov PS. Efficacy of omalizumab in delayed pressure urticaria: a case report. Allergy 2010; 65: 138–9. DOI: 10.1111/j.1398-9995.2009.02188.x. PubMed
- Marin-Cabanas I, Berbegal de Gracia L, de Leon-Marrero F, Hispan P, Silvestre JF. Management of chronic spontaneous urticaria in routine clinical practice following the EAACI/GA(2) LEN/EDF/WAO guidelines. Actas Dermo-Sifiliograficas 2017; 108(4): e27–e32. DOI: 10.1016/j.adengl.2017.03.014. Journal
On DermNet
- Urticaria — an overview
- Angioedema
- Anaphylaxis
- Urticaria in children
- Urticaria and urticaria-like conditions
- Food allergy
- Contact urticaria
- Cholinergic urticaria
- Cold urticaria
- Drug-induced urticaria
- Heat urticaria
- Aquagenic urticaria
- Vibratory urticaria
- Vibratory angioedema
- Dermographism
- Delayed pressure urticaria
- Solar urticaria
- Serum sickness
- Serum sickness-like reaction
- Dermatological emergencies CME
- Autologous serum skin testing
- Exercise-induced anaphylaxis
- Skin signs of rheumatic disease
Other websites
- Hives — MedlinePlus
- AllAllergy.Net — Allergy and intolerance information resource
- Chronic urticaria — Medscape
- Hives and angioedema — emedicinehealth
- Urticaria and angioedema — British Association of Dermatologists [patient information leaflet]
- Patient education: Hives (urticaria) (Beyond the Basics) — UpToDate
- Urticaria Control Test (PDF)
- eProvide
