Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Blue toe syndrome — extra information
Blue toe syndrome
Author: Catherine Tian, Medical Student, Department of Dermatology, University of Auckland, Auckland, New Zealand. Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. November 2018.
Introduction
Causes
Clinical features
Complications
Diagnosis
Treatment
What is blue toe syndrome?
Blue toe syndrome, also known as occlusive vasculopathy, is a form of acute digital ischaemia in which one or more toes become a blue or violet colour. There may also be scattered areas of petechiae or cyanosis of the soles of the feet.
Blue toe syndrome is associated with small vessel occlusion and can occur without obvious preceding trauma or disorders that produce generalised cyanosis, such as hypoxaemia or methaemoglobinaemia [1]. It most often presents in an older man who has undergone a vascular procedure.

Blue toe syndrome: ischaemia

What causes blue toe syndrome?
The characteristic blue discolouration and pain in blue toe syndrome are caused by impaired blood flow to the tissue resulting in ischaemia. The impairment of blood flow is due to one or more of the following factors:
- Decreased arterial flow
- Impaired venous outflow
- Abnormalities in circulating blood.
These are not mutually exclusive. For example, abnormal circulating blood can induce vasculitis and subsequent thrombosis of the arterioles and capillaries supplying blood to the toes, resulting in a decreased arterial flow.
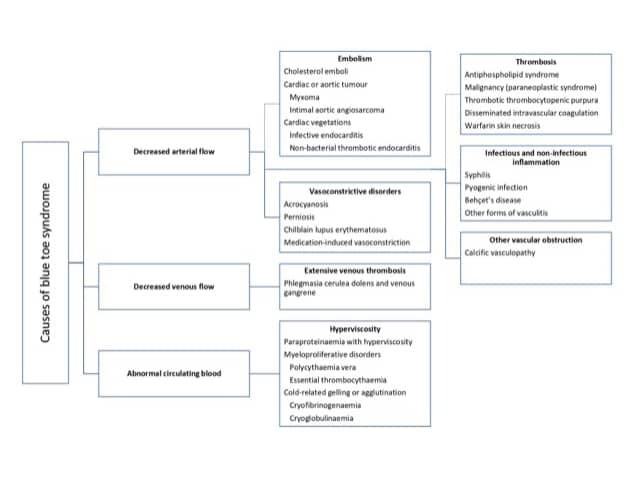
Adapted from Hirschmann JV, Raugi GJ. J Am Acad Dermatol 2009
Decreased arterial flow
The blockage or narrowing of arteries by the small clots that lead to blue toe syndrome can result from a number of different conditions.
Embolisation
- Cholesterol emboli are cholesterol fragments or fibrin–platelet material released into the bloodstream from ulcerated arteriosclerotic plaques in the large arteries (eg, the aorta, and the iliac and femoral arteries) and are the most common cause of blue toe syndrome. Risk factors include smoking, hypertension, elevated cholesterol levels, and a recent angiogram or vascular surgery.
- Embolisation (formation of an embolus, a floating mass in the bloodstream that can clog the arteries) can also occur spontaneously [2].
- Emboli may originate from a cardiac tumour or from vegetations (clots or growths made of fibrin and blood platelets) from a cardiac myxoma or endocarditis (septic emboli). It is rare that an embolus will develop without any apparent cardiovascular risk factors or a precipitating event [3].
Thrombosis
- Thrombosis can form in the small vessels of the feet.
- It can result from the antiphospholipid syndrome, thromboangiitis obliterans, malignancy, thrombotic thrombocytopenic purpura, disseminated intravascular coagulation, and warfarin-induced skin necrosis [1].
Vasoconstrictive disorders
- Narrowing of blood vessels in the feet can be a result of muscular wall contraction.
- In Raynaud disease, vasoconstriction tends to affect multiple fingers more severely than the toes.
- Causes include medication-induced vasoconstriction (eg, a beta-blocker or illicit drug such as cocaine) and/or acrocyanosis [1].
Infectious and non-infectious inflammation
Occlusion can also be due to syphilis, pyogenic infection (sepsis), Behçet disease, and other forms of vasculitis [1,4].
Other causes of vascular obstruction
Narrowed blood vessels can be due to calcific vasculopathy (calciphylaxis) [5].
Impaired venous outflow
Abnormal venous drainage associated with extensive venous thrombosis results in phlegmasia cerulea dolens (a painful form of blue toe syndrome associated with leg oedema). Many patients have predisposing factors for venous thrombosis, including:
- Immobility
- Clotting disorders
- Pregnancy
- Previous leg trauma
- Malignancy [6].
Abnormalities in circulating blood
Blue toe syndrome can be due to abnormal blood constituents. See the DermNet page on Skin conditions of haematological disorders.
- Platelet plugging
- Myeloproliferative disorders (eg, polycythaemia rubra vera and essential thrombocythaemia)
- Paraproteinaemia (which causes hyperviscosity)
- Cryoglobulinaemia
- Cryofibrinogenaemia
- Cold agglutinin anaemia
- Paroxysmal nocturnal haemoglobinuria [7]
What are the clinical features of blue toe syndrome?
The clinical features of blue toe syndrome can range from an isolated blue and painful toe to a diffuse multi-organ system disease that can mimic other systemic illnesses. Any organ or tissue can be affected, although the skin and skeletal muscles of the lower extremities are almost always involved [8].
Cutaneous abnormalities are usually one of the earliest symptoms; most commonly, blue or purple discolouration of the affected toes [9]. Discolouration may affect one foot or both, depending on the underlying pathophysiology. It is often painful and may be associated with claudication.
In a series of 223 patients with cholesterol embolisation, the most frequent cutaneous findings were:
- Livedo reticularis or livedo racemosa (in 49% of the patients with skin manifestations)
- Gangrene (35%)
- Acrocyanosis (28%)
- Ulceration (17%)
- Nodules (10%)
- Purpura (9%).
Livedo reticularis may be non-blanching or blanching when the discolouration disappears with pressure and/or fades with leg elevation [10]. Blanching occurs in the first stages of blue toe syndrome, as the sluggish flow of desaturated blood results in the temporary obstruction of blood flow [1].
- Pain in the affected blue toe or toes is usually of acute onset and occurs at rest. The non-discoloured areas of the foot and distal limb can also be painful [11].
- The affected toes are cold compared to unaffected parts of the foot, which are warmer and appear well-perfused [6]. Foot pulses may be normal.
- Peripheral foot pulses may be palpable if an occlusion occurs in the small arteries and arterioles rather than in large palpable arteries [6].
What are the complications of blue toe syndrome?
Mild forms of blue toe syndrome have a good prognosis and subside without sequelae [1]. However, cholesterol fragments blocking blood vessels to other organs can lead to multi-organ disorder [1]. Involvement of the kidneys has a poor prognosis.
Patients with untreated blue toe syndrome from embolisation can suffer from further emboli in the subsequent weeks, resulting in substantial occlusion and the ischaemic loss of digits, the forefoot, and the limb (dry gangrene), necessitating amputation [6].
How is blue toe syndrome diagnosed?
Blue toe syndrome is a clinical diagnosis based on patient history and findings on examination. It is important to determine the underlying cause of blue toe syndrome to guide treatment [1]. There are usually clues from the clinical assessment, but to confirm the diagnosis, investigation in the form of laboratory blood works, tissue biopsies, and radiological imaging is required.
History and examination should focus on:
- Hypertension or other risk factors for hypercholesterolaemia and atherosclerotic diseases
- Fever (indicating cholesterol emboli, infective endocarditis, myxoma, thrombotic thrombocytopenic purpura, and disseminated intravascular coagulation)
- Cardiac murmur (infective endocarditis and atrial myxoma)
- Livedo reticularis (cholesterol emboli, myxoma, antiphospholipid syndrome, hyperviscosity syndrome, cryofibrinogenaemia, cryoglobulinaemia, and calciphylaxis)
- Extensive oedema in the ipsilateral leg (phlegmasia cerulean dolens)
- Hollenhorst plaques (cholesterol emboli) noted on retinal examination
- Dilated veins, haemorrhages, and exudates in retinal examination (hyperviscosity syndrome) [1–3].
A full blood count including a white cell differential, erythrocyte sedimentation rate, and C-reactive protein may indicate elevated inflammatory markers. These are often non-specific in blue toe syndrome and can occur with cholesterol emboli as well as numerous other inflammatory driven processes. The blood count and peripheral blood film can help diagnose bone marrow or autoimmune diseases. Liver and renal functions should also be checked.
Other more specific blood tests may include:
- Coagulation tests for disseminated intravascular coagulation
- Antinuclear antibodies
- Antiphospholipid antibodies
- Blood cultures (for suspected septic emboli)
- Haemolysis screen
- Cold agglutinins
- Cryofibrinogen level
- Cryoglobulin level
- Serum and urine protein electrophoresis and immunofixation
- Hepatitis C (for suspected cryoglobulinaemia)
- Syphilis serology [1].
Imaging may include:
- A chest radiograph and/or thoracic and abdominal computed tomography or magnetic resonance imaging to look for any aortic atheroma and underlying cancer in malignancy-associated conditions
- A peripheral angiogram and a scan of the limb arteries (to locate vessel narrowing, occlusion, and/or determine the source of emboli)
- Sonography of the abdomen and a venous duplex ultrasound scan to detect deep venous thrombosis
- An echocardiogram to detect cardiac tumours or vegetations from endocarditis [1,12].
A definitive diagnosis is usually made by the histopathological confirmation of a biopsy of the affected skin or other involved tissues [13]. Biopsies in patients with a poor peripheral vascular supply should be performed with caution as poor healing is likely at the sampling site. The histopathological findings for cholesterol emboli show intravascular cholesterol crystals, which may be associated with macrophages, giant cells, and eosinophils [13].
What is the treatment for blue toe syndrome?
The principles of treatment revolve around addressing the cause of the blue toe syndrome. This is usually in the form of relieving occlusion and restoring arterial or venous vessel continuity [6].
- Medical anticoagulation (especially antiplatelet drugs), and surgical endovascular or reconstructive procedures are indicated for emboli and thromboses, to remove the source of the clot, resolve occlusion, and restore blood flow.
- Haematological treatment may be required when blue toe syndrome is due to hyperviscosity [14].
- Supportive and symptomatic treatments of blue toe syndrome include rest, warm conditions, appropriate dressings, and hydration [14].
Address patient risk factors
Risk factors should be addressed in patients with advanced atherosclerotic disease, including:
- Smoking cessation
- Control of hypertension
- Reduction of serum cholesterol.
Patients with stenotic lesions should be followed up carefully, as the progression of the atheromatous disease will result in a strong likelihood of repetition of the blue toe syndrome [6].
References
- Hirschmann JV, Raugi GJ. Blue (or purple) toe syndrome. J Am Acad Dermatol 2009; 60: 1–20. DOI: 10.1016/jaad.2008.09.038. PubMed
- O’Keeffe ST, Woods BO, Breslin DJ, Tsapatsaris NP. Blue toe syndrome: causes and management. Arch Intern Med 1992; 152: 2197–202. PubMed
- Hoffmeier A, Sindermann JR, Scheld HH, Martens S. Cardiac tumours — diagnosis and surgical treatment. Dtsch Arztebl Int 2014; 111: 205–11. DOI: 10.3238/arztebl.2014.0205. PubMed Central
- Federman DG, Valdivia M, Kirsner RS. Syphilis presenting as the 'blue toe syndrome'. Arch Intern Med 1994; 154: 1029–31. PubMed
- Guldbakke KK, Khachemoune A. Calciphylaxis. Int J Dermatol 2007; 46: 231–8. DOI: 10.111/j.1365-4632.2007.03160.x. PubMed
- Karmody AM, Powers SR, Monaco VJ, Leather RP. "Blue toe" syndrome. An indication for limb salvage surgery. Arch Surg 1976; 111: 1263–68. DOI: 10.1001/archsurg.1976.01360290097015. PubMed
- Kealy WF. Atheroembolism. J Clin Pathol 1978; 31: 984–9. PubMed Central
- Davis MD, Dy KM, Nelson S. Presentation and outcome of purpura fulminans associated with peripheral gangrene in 12 patients at Mayo Clinic. J Am Acad Dermatol 2007; 57: 944–56. DOI: 10.1016/j.jaad.2007.07.039. PubMed
- Jucgla A, Moreso F, Muniesa C, Moreno A, Vidaller A. Cholesterol embolism: still an unrecognised entity with a high mortality rate. J Am Acad Dermatol 2006; 55: 786–93. DOI: 10.1016/j.jadd.2006.05.012. PubMed
- Falanga V, Fine MJ, Kapoor WN. The cutaneous manifestations of cholesterol crystal embolization. Arch Dermatol 1986; 122: 1194–8. DOI: 10.1001/archderm.1986.01660220112024. PubMed
- Scolari F, Ravani P, Gaggi R, et al. The challenge of diagnosing atheroembolic renal disease: clinical features and prognostic factors. Circulation 2007; 116: 298–304. DOI: 10.1161/CIRCULATIONAHA.106.680991. PubMed
- Poredos P. Poredos P. Blue toe syndrome. European Society of Cardiology E-Journal of Cardiology Practice 2004; 2 (18). Journal
- Llamas-Velasco M, Alegría V, Santos-Briz Á, Cerroni L, Kutzner H, Requena L. Occlusive nonvasculitic vasculopathy. Am J Dermatopathol 2017; 39: 637–662. DOI: 10.1097/dad.0000000000000766. PubMed
- Vayssairat M, Chakkour K, Gouny P, Nussaume O. [Atheromatous embolisms and cholesterol embolisms: medical treatment]. J Mal Vasc 1996; 21 (Suppl A): 97–9. [Article in French] PubMed
On DermNet
Other websites
- Dermatological emergencies — DermNet e-lecture [Youtube]
- Blue toe syndrome — European Society of Cardiology E-Journal of Cardiology Practice (2004)
