Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lichen sclerosus — extra information
Lichen sclerosus
Author: Dr Amanda Oakley, Dermatologist, Website Manager, Chief Editor, Hamilton, New Zealand, 1997. Updated January 2016.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Treatment
Outlook
What is lichen sclerosus?
Lichen sclerosus is a common chronic inflammatory skin disorder that most often affects genital and perianal areas.
Older names for lichen sclerosus include lichen sclerosus et atrophicus, kraurosis vulvae (in women), and balanitis xerotica obliterans (in males).


Who gets lichen sclerosus?
Lichen sclerosus can start at any age, although it is most often diagnosed in women over 50. Pre-pubertal children can also be affected.
- Lichen sclerosus is ten times more common in women than in men. [see Lichen sclerosus in men]
- 15% of patients know of a family member with lichen sclerosus.
- It may follow or co-exist with another skin condition, most often lichen simplex, psoriasis, erosive lichen planus, vitiligo, or morphoea.
- People with lichen sclerosus often have a personal or family history of another autoimmune disease such as thyroid disease (about 20% of patients), pernicious anaemia, or alopecia areata.
What causes lichen sclerosus?
The cause of lichen sclerosus is not fully understood and may include genetic, hormonal, irritant, traumatic, and infectious components.
Lichen sclerosus is often classified as an autoimmune disease. Autoimmune diseases are associated with antibodies to a specific protein.
- Extracellular matrix protein-1 (ECM-1) antibodies have been detected in 60–80% of women with vulval lichen sclerosus.
- Antibodies to other unknown proteins may account for other cases, explaining differing presentations of lichen sclerosus and response to treatment.
- However, these antibodies could be epigenetic, ie, the results of disease rather than the cause of disease.
Male genital lichen sclerosus is rare in men circumcised in infancy. It has been suggested that it may be caused by chronic, intermittent damage by urine occluded under the foreskin.
As onset in women is commonly postmenopausal, a relative lack of oestrogen may be significant.
What are the clinical features of lichen sclerosus?
Lichen sclerosus presents as white crinkled or thickened patches of skin that tend to scar.
Vulval lichen sclerosus
Lichen sclerosus primarily involves the non-hair bearing, inner areas of the vulva.
- It can be localised to one small area or extensively involve perineum, labia minora (inner lips) and clitoral hood.
- It can spread onto the surrounding skin of the labia majora and inguinal fold and, in 50% of women, to the anal and perianal skin.
- Lichen sclerosus never involves vaginal mucosa.
Lichen sclerosus can be extremely itchy and sore (see Pruritus vulvae).
- Sometimes bruises, blood blisters and ulcers appear after scratching, or from minimal friction (eg, tight clothing, sitting down).
- Urine can sting and irritate.
- Sexual intercourse can be very uncomfortable and may result in painful fissuring of the posterior fourchette at the entrance to the vagina.
- It may cause discomfort or bleeding when passing bowel motions, and aggravate any tendency to constipation, particularly in children.
Lichen sclerosus causes adhesions and scarring.
- The clitoris may be buried.
- The labia minora resorb/shrink.
- The entrance to the vagina tightens (introital stenosis).
See Vulval lichen sclerosus images.
See Perianal lichen sclerosus images.
See Anogenital lichen sclerosus in skin of colour images.
Penile lichen sclerosus
In men, lichen sclerosus usually affects the tip of the penis (glans), which becomes white, firm and scarred. [see Lichen sclerosus in men]
- The urethra may narrow (meatal stenosis), resulting in a thin or crooked urinary stream.
- The foreskin may become difficult to retract (phimosis).
- Sexual function may be affected, because of painful erections or embarrassment.
See Images of penile lichen sclerosus.
See Anogenital lichen sclerosus in skin of colour images.
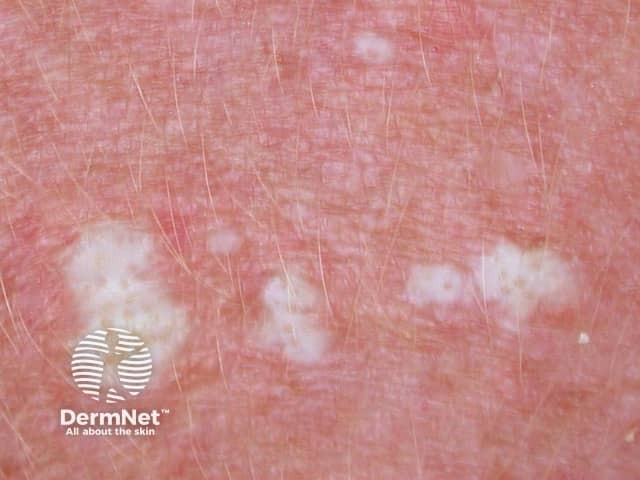
Extragenital lichen sclerosus
Extragenital lichen sclerosus refers to lichen sclerosus at other sites.
- Extragenital lichen sclerosus affects 10% of women with the vulval disease.
- Only 6% of men and women with extragenital lichen sclerosus do not have genital lichen sclerosus at the time of diagnosis.
One or more white dry plaques may be found on the inner thigh, buttocks, lower back, abdomen, under the breasts, neck, shoulders, and armpits.
- Lichen sclerosus resembles cigarette paper, as the skin is dry, wrinkled and thin (atrophic).
- Hair follicles may appear prominent, containing dry plugs of keratin.
- Bruises, blisters and ulcers may appear without noticeable trauma.


Axillary lichen sclerosus

See more on Extragenital lichen sclerosus images.
What are the complications of lichen sclerosus?
Infections
Patients with lichen sclerosus may develop infections, particularly Candida albicans, herpes simplex, Staphylococcus aureus. Herpes infections are particularly painful and may cause vulval ulceration.
Squamous cell carcinoma
Lichen sclerosus of anogenital sites is associated with an increased risk of vulval, penile or anal cancer (squamous cell carcinoma, SCC).
- Cancer is estimated to affect up to 5% of patients with vulval lichen sclerosus.
- Cancer is more likely if the inflammatory disease is uncontrolled.
- Invasive SCC presents as an enlarging lump or a sore that fails to heal.
- High-grade squamous intraepithelial lesions in females (SIL) or males associated with lichen sclerosus may be HPV-associated (usual type) or differentiated.
Extragenital lichen sclerosus does not appear to predispose to cancer.
How is lichen sclerosus diagnosed?
An experienced clinician can often diagnose lichen sclerosus by its appearance. Dermoscopy can provide further clues. Skin biopsy is frequently recommended.
- Histopathology may confirm the suspected diagnosis of lichen sclerosus.
- Another skin condition may be diagnosed or coexist with lichen sclerosus.
- A focal area may undergo a biopsy to assess for cancer or SIL.
A biopsy may also be recommended at follow-up, to evaluate areas of concern or to explain the inadequate response to treatment.
What is the treatment for lichen sclerosus?
Patients with lichen sclerosus are best to consult a doctor with a particular interest in the condition for accurate diagnosis and treatment recommendations.
They are advised to become familiar with the location and appearance of their lichen sclerosus.
- Women may use a mirror when applying topical therapy.
- Photographs may help in monitoring activity and treatment.
General measures for genital lichen sclerosus
- Wash gently once or twice daily.
- Use a non-soap cleanser, if any.
- Try to avoid tight clothing, rubbing and scratching.
- Activities such as riding a bicycle or horse may aggravate symptoms.
- If incontinent, seek medical advice and treatment.
- Apply emollients to relieve dryness and itching, and as a barrier to protect sensitive skin in genital and anal areas from contact with urine and faeces.
Topical steroid ointment
Topical steroids are the primary treatment for lichen sclerosus. An ultrapotent topical steroid is often prescribed (eg, clobetasol propionate 0.05%). A potent topical steroid (eg, mometasone furoate 0.1% ointment) may also be used in mild disease or when symptoms are controlled.
- An ointment base is less likely than cream to sting or to cause contact dermatitis.
- A thin smear should be precisely applied to the white plaques and rubbed in gently.
- Most patients will be told to apply the steroid ointment once a day. After one to three months (depending on the severity of the disease), the ointment can be used less often.
- Topical steroid may need to be continued once or twice a week to control symptoms or to prevent lichen sclerosus recurring.
- Itch often settles within a few days, but it may take weeks to months for the skin to return to normal (if at all).
- One 30-g tube of topical steroid should last 3 to 6 months or longer.
The doctor should reassess the treated area after a few weeks, as a response to treatment is quite variable.
Topical steroids are safe when used appropriately. However, excessive use or application to the wrong site can result in adverse effects. In anogenital areas, these include:
- Red, thin skin
- Burning discomfort
- Periorificial dermatitis
- Candida albicans infection (eg, vulvovaginal thrush)
It is most important to follow instructions carefully and to attend follow-up appointments regularly.
Other topical therapy
Other topical treatments used in patients with lichen sclerosus include:
- Intravaginal oestrogen cream or pessaries in postmenopausal women. These reduce symptoms due to atrophic vulvovaginitis (dry, thin, fissured and sensitive vulval and vaginal tissues due to hormonal deficiency).
- Topical calcineurin inhibitors tacrolimus ointment and pimecrolimus cream instead of or in addition to topical steroids. They tend to cause burning discomfort (at least for the first few days). Early concern that these medications may have the potential to accelerate cancer growth in the presence of oncogenic human papillomavirus (the cause of genital warts) appears unfounded.
- Topical retinoid (eg, tretinoin cream) is not well tolerated on genital skin but may be applied to other sites affected by lichen sclerosus. It reduces scaling and dryness.
Oral medications
When lichen sclerosus is severe, acute, and not responding to topical therapy, systemic treatment may rarely be prescribed. Options include:
- Intralesional or systemic corticosteroids
- Oral retinoids: acitretin, isotretinoin
- Methotrexate
- Ciclosporin
Surgery
Surgery is essential for high-grade squamous intraepithelial lesions or cancer.
In males, circumcision is effective in lichen sclerosus affecting prepuce and glans of the penis. It is best done early if initial topical steroids have not controlled symptoms and signs. If the urethra is stenosed or scarred, reconstructive surgery may be necessary.
In females, the release of vulval and vaginal adhesions and scarring from vulval lichen sclerosus may occasionally be performed to reduce urination difficulties and allow intercourse if dilators have not proved effective. Procedures include:
- Simple perineotomy (a division of adhesions)
- Fenton procedure (an incision that is repaired transversely)
- Perineoplasty (excision of involved tissue and vaginal mucosal advancement)
Unfortunately, lichen sclerosus sometimes closes up the vaginal opening again after surgery has initially appeared successful. It can be repeated.
Other treatments
Other reported treatments for lichen sclerosus are considered experimental at this time.
- CO2 laser ablation of hyperkeratotic plaques
- Er:YAG laser
- Phototherapy
- Photodynamic therapy
- Fat injections
- Stem cell and platelet-rich plasma injections
What is the outlook for lichen sclerosus?
Lichen sclerosus is a chronic disease and usually persists for years.
- Extragenital lichen sclerosus is more likely than anogenital disease to clear.
- Early treatment occasionally leads to complete and long-term remission.
- Scarring is permanent.
Long-term follow-up is recommended to monitor the disease, optimise treatment and ensure early diagnosis of cancer.
References
- Bunker CB, Shim TN. Male genital lichen sclerosus. Indian J Dermatol. 2015 Mar-Apr;60(2):111-17. doi: 10.4103/0019-5154.152501. Review. PubMed PMID: 25814697; PubMed Central PMCID: PMC4372901.
- Casabona F, Priano V, Vallerino V, Cogliandro A, Lavagnino G. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plastic and Reconstructive Surgery. 126(4):210e-11e. doi: 10.1097/PRS.0b013e3181ea9386 Journal
- Neill SM, Lewis FM, Tatnall FM, Cox NH; British Association of Dermatologists. British Association of Dermatologists' guidelines for the management of lichen sclerosus 2010. Br J Dermatol. 2010;163(4):672-82. doi:10.1111/j.1365-2133.2010.09997.x PubMed
- Kirtschig G, Becker K, Günthert A, et al. Evidence-based (S3) Guideline on (anogenital) Lichen sclerosus. J Eur Acad Dermatol Venereol. 2015;29(10):e1-e43. doi:10.1111/jdv.13136 Journal
- Gómez-Frieiro M, Laynez-Herrero E. Use of Er:YAG laser in the treatment of vulvar lichen sclerosus. Int J Womens Dermatol. 2019;5(5):340-4. doi:10.1016/j.ijwd.2019.05.007 Journal
- Kirtschig G. Lichen sclerosus-presentation, diagnosis and management. Dtsch Arztebl Int. 2016;113(19):337-43. doi:10.3238/arztebl.2016.0337 Journal
- Orszulak D, Dulska A, Niziński K, et al. Pediatric vulvar lichen sclerosus-a review of the literature. Int J Environ Res Public Health. 2021;18(13):7153. doi:10.3390/ijerph18137153 Journal
- Chi CC, Kirtschig G, Baldo M, Brackenbury F, Lewis F, Wojnarowska F. Topical interventions for genital lichen sclerosus. Cochrane Database Syst Rev. 2011;2011(12):CD008240. doi:10.1002/14651858.CD008240.pub2. PubMed
On DermNet
- Lichen sclerosus in men
- Lichen sclerosus pathology
- Dermoscopy of lichen sclerosus
- Genital skin conditions
- Pruritus vulvae
- Scleroderma
- Vulval cancer
- Vulval intraepithelial neoplasia (SIL, VIN)
- Erosive lichen planus
- Lichenoid disorders
- Vulval cancer
Other websites
- ISSVD Vulvovaginal Disorders: an algorithm for basic adult diagnosis and treatment
- Vulvovaginal Disorders: A Pathway to Diagnosis and Treatment
- Lichen Sclerosus (females) — British Association of Dermatologists
- Lichen Sclerosus (males) — British Association of Dermatologists
- Lichen sclerosus: the unspoken pain on Vimeo — Dr Andrew Goldstein talks about lichen sclerosus in a video presentation (1 hour 20 mins)
- Worldwide Lichen Sclerosus Support
- Supportgroep and Stichting Lichen Sclerosus Nederland
- Scratch Sclerosus quartet game, in Dutch, but soon to be made available in English
