Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Hand dermatitis — extra information
Hand dermatitis
Author: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1997. Updated by Dr Karen Koch, Consultant Dermatologist, Donald Gordon Medical Clinic, University of the Witwatersrand, Johannesburg, South Africa. March 2018. Minor update by Ian Coulson, Dermatologist. Copy edited by Gus Mitchell. July 2024.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outlook
What is hand dermatitis?
Hand dermatitis is a common acute or chronic eczematous disorder that affects the dorsal and palmar aspects of the hands due to a variety of causes.
Hand dermatitis is also known as hand eczema.

Palmar dermatitis

Hyperkeratotic palmar eczema

Thickening, dryness, and scale on the dorsal fingers
See more images of hand dermatitis.
Who gets hand dermatitis?
Hand dermatitis is common, especially in young adult females, and accounts for 20–35% of all forms of dermatitis. It may occur at any age, including during childhood. It is particularly prevalent in people with a history of atopic dermatitis. [see also Atopic hand dermatitis]
Chronic hand dermatitis is estimated to affect 10–15% of the population and is a common cause of time lost from work.
Hand dermatitis is particularly common in industries involving wet work or exposure to chemicals such as cleaning, catering, metalwork, hairdressing, healthcare, housework, construction, painting and mechanical work. This is mainly due to contact with irritants, but specific contact allergies can contribute [2].
What causes hand dermatitis?
Hand dermatitis often results from a combination of causes, including:
- Genetic and unknown factors (constitutional hand dermatitis)
- Injury (contact irritant dermatitis)
- Immune reactions (allergic contact dermatitis).
Hand dermatitis is frequently caused or aggravated by work when it is known as occupational dermatitis.
Irritants include water, detergents, solvents, acids, alkalis, cold, heat, friction, and desiccating dusts. These can damage the outer stratum corneum, removing lipids and disturbing the skin’s barrier function. Water loss and inflammation lead to further impairment of barrier function.
In atopic dermatitis, a deficiency in or defective function of the filaggrin protein in the stratum corneum leads to barrier dysfunction resulting in water loss and easy penetration by irritants and allergens [3].
Contact allergy is a delayed hypersensitivity reaction with elicitation and memory phases involving T lymphocytes and release of cytokines [2].
What are the clinical features of hand dermatitis?
Hand dermatitis may affect the backs of the hands, the palms, or both. It can be very itchy, often with a burning sensation, and is sometimes painful. It has acute, relapsing, and chronic phases.
Acute hand dermatitis presents with:
- Red macules, papules, and plaques
- Swelling
- Blistering, weeping, crusting
- Fissuring.
Features of chronic hand dermatitis include:
- Dryness and scale
- Lichenification.
There are various causes and clinical presentations of hand dermatitis.

Diffuse scale and redness on the palms due to eczema

Infected hand dermatitis

Hand dermatitis on the dorsal fingers in an atopic boy
Atopic hand dermatitis
Atopic hand dermatitis is due to impaired skin barrier function and is triggered by contact with irritants. It usually involves the backs of the hands and around the wrists. It may manifest as a discoid or vesicular pattern of eczema. Patients will typically have signs of atopic dermatitis elsewhere such as in the flexures.
Discoid eczema
Discoid eczema (nummular dermatitis) tends to affect the dorsal surfaces of the hands and fingers as circumscribed plaques. Other sites of the body may or may not be affected.
Vesicular hand dermatitis
Vesicular hand dermatitis is also known as pompholyx. Intensely itchy crops of skin-coloured blisters arise on the palms and the sides of the hands and fingers. Similar symptoms often affect the feet. It is likely this form of dermatitis is exacerbated by excessive sweating (hyperhidrosis) such as in hot and/or humid weather and with emotional stress.
Chronic relapsing vesiculosquamous dermatitis
Chronic relapsing vesiculosquamous dermatitis is a common pattern of palmar and finger dermatitis, in which episodes of acute vesicular dermatitis are followed by chronic scaling and fissuring.
Hyperkeratotic hand dermatitis
Hyperkeratotic hand dermatitis is a chronic, dry, non-inflammatory palmar dermatitis. It can appear similar to palmar psoriasis but is less red and less well circumscribed.
Fingertip dermatitis
Fingertip dermatitis can be isolated to one or several fingers.
Irritant contact dermatitis
The hands are the most common site for irritant contact dermatitis and are often due to wet work and repeated exposure to low-grade irritants. The finger-webs are the first place to be affected, but inflammation can extend to fingers, the backs of the hands and the wrists. Irritant contact dermatitis often spares the palms.
- Acute irritant contact dermatitis is due to injury by potent irritants such as acids and alkalis, often in an occupational setting.
- Repeated exposure to low-grade irritants such as water, soaps, and detergents leads to chronic cumulative irritant dermatitis.
Allergic contact dermatitis
Allergic contact dermatitis may be difficult to distinguish from constitutional forms of hand dermatitis and irritant contact dermatitis. There are about 30 common allergens and innumerable uncommon or rare ones that may affect the hands. Common allergens include nickel, fragrances, rubber accelerators and chromate (in gloves), and p-phenylenediamine (permanent hair-dye). Clues to contact allergy depend on the allergen, but may include:
- Periodic flare-ups associated with certain tasks or places hours to days earlier
- Irregular, asymmetrical distribution of the rash
- Sharp border to the rash (eg, at the wrist, corresponding with the cuff of rubber glove).
What are the complications of hand dermatitis?
- Bacterial skin infections (staphylococci and/or streptococci) can result in pustules, crusting, pain, and even limb lymphoedema.
- Dermatitis at the ends of the fingers may result in deformed nails.
- Dermatitis can spread to affect other sites, particularly the forearms and feet.
How is hand dermatitis diagnosed?
Hand dermatitis is usually straightforward to diagnose and classify by history and examination, considering:
- Acute, relapsing, or chronic course
- Past history of skin disease
- Dermatitis on other sites
- Occupation and hobbies.
However determining the cause of a hand dermatitis can be complicated as it may be multifactorial.
Patients with chronic hand dermatitis may require patch tests to detect contact allergens.
A punch biopsy and skin scrapings (mycology) may be necessary to exclude other causes of inflammation of the hands.
What is the differential diagnosis for hand dermatitis?
- Contact urticaria — for example, to latex gloves (generally results in immediate redness, itching and swelling that resolves within an hour)
- Protein contact dermatitis, most often affecting caterers (a combination of urticaria and dermatitis induced by reactions to meat)
- Psoriasis (symmetrical, well-circumscribed, red, scaly plaques)
- Tinea manuum (unilateral or asymmetrical, peripheral scale).

Applying patch tests to the back

Reading the patch tests - there are several positives
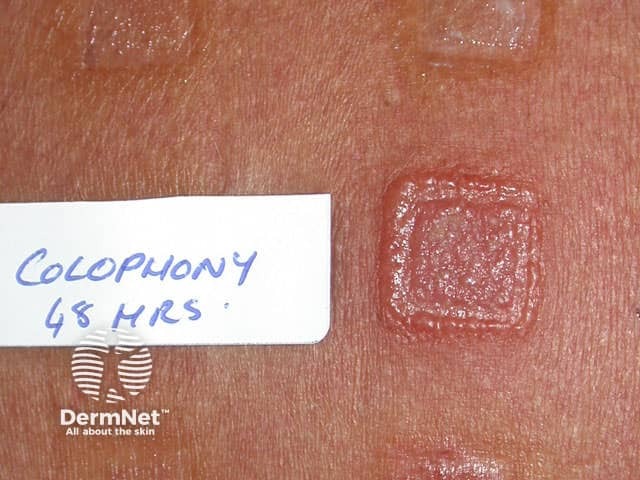
Positive patch test reaction
What is the treatment for hand dermatitis?
Patients with all forms of hand dermatitis should be most particular to:
- Minimise contact with irritants — even water
- Use non-soap cleanserwhen washing hands, rinse carefully, and ensure hands are completely dry afterwards
- Note that cream cleansers are not antimicrobial; soap and water or a sanitiser is needed for washing hands in order to destroy pathogens such as the SARS-CoV-2 virus responsible for COVID-19
- Completely avoid allergens that have been identified by patch testing
- Wear task-appropriate protective gloves
- Apply thick emollients before work/school and reapply after washing or when the skin dries out (this can be 10–20 times in a day).
Vinyl gloves are less likely than rubber gloves to cause allergic reactions.
- They must be scrupulously clean and should have no holes.
- They should not be worn for long periods.
- Sweating under the gloves aggravates dermatitis.
- Lined gloves or inner cotton gloves improve comfort.
- Cotton gloves may be useful for irritating dry work when a waterproof outer glove is not required.
Topical steroids reduce inflammation.
- Use a potent topical steroid on dermatitis on the backs of the hands and an ultrapotent topical steroid on palms.
- Cream formulation is usually best for vesicular hand dermatitis, and an ointment base for chronic dermatitis.
- They should be applied to areas of active dermatitis once or twice daily for several weeks, then discontinued or frequency/potency reduced.
- Short-term occlusion increases potency and is warranted if standard applications have not been effective.
Calcineurin inhibitors (tacrolimus and pimecrolimus) have some evidence to show efficacy in hand eczema and can be used as a steroid-sparing agent [4].
Delgocitanib is a topical pan JAK inhibitor in a topical formulation that has been shown to reduce the signs and symptoms of chronic hand eczema. It is awaiting NICE approval in the UK.
Alitretinoin has been approved for recalcitrant hand dermatitis in some countries.
Secondary bacterial infection may require an oral antibiotic, usually flucloxacillin.
Severe acute flares of hand dermatitis are treated with short course oral prednisone (systemic steroids) for 2–4 weeks.
Chronic intractable hand dermatitis may be treated with second-line agents such as azathioprine, methotrexate, ciclosporin, alitretinoin or phototherapy.
How can hand dermatitis be prevented?
Contact irritant hand dermatitis can be prevented by careful protective measures and active treatment. It is very important that people with atopic dermatitis are aware of the risk of hand dermatitis, particularly when considering an occupation.
What is the outlook for hand dermatitis?
With careful management, hand dermatitis usually recovers completely. A few days off work may be helpful. When occupational dermatitis is severe, it may not be possible to work for weeks or months. Occasionally a change of occupation is necessary.
References
- Thyssen JP, Johansen JD, Linneberg A, Menne T. The epidemiology of hand eczema in the general population--prevalence and main findings. Contact Dermatitis. 2010;62(2):75–87. PubMed
- Perry AD, Trafeli JP. Hand dermatitis: review of etiology, diagnosis, and treatment. J Am Board Fam Med. 2009;22(3):325–30. PubMed
- McLean WH. Filaggrin failure - from ichthyosis vulgaris to atopic eczema and beyond. Br J Dermatol. 2016;175 Suppl 2:4–7. PubMed
- Raja S, Raja A, Shuja MH, Ali A. Clinical benefits of delgocitinib cream for chronic hand eczema: a systematic review and meta-analysis. Arch Dermatol Res. 2024;316(10):734. PubMed
- Schliemann S, Kelterer D, Bauer A,et al. Tacrolimus ointment in the treatment of occupationally induced chronic hand dermatitis. Contact Dermatitis. 2008;58(5):299–306. PubMed
- Worm M, Thyssen JP, Schliemann S, et al. The pan-JAK inhibitor delgocitinib in a cream formulation demonstrates dose response in chronic hand eczema in a 16-week randomized phase IIb trial. Br J Dermatol. 2022;187(1):42–51. PubMed
- Raja S, Raja A, Shuja MH, Ali A. Clinical benefits of delgocitinib cream for chronic hand eczema: a systematic review and meta-analysis. Arch Dermatol Res. 2024;316(10):734. Published 2024 Nov 1. PubMed
On DermNet
- Dermatitis
- Fingertip dermatitis
- Atopic hand dermatitis
- Images of hand dermatitis
- Allergic contact dermatitis
- Irritant contact dermatitis
- Gloves for hand protection
- Hand care in healthcare workers
- Emollients for eczema
- Pompholyx
- Hyperkeratotic palmar dermatitis
- Nummular dermatitis
- Patch testing
- Dermatitis online course for health professionals
- Occupational skin disorders in homemakers
- Treatment of psychodermatological disorders
- Occupational dermatitis among construction workers
- Occupational skin disorders in homemakers
Other websites
- Hand eczema — Occupational Dermatology Research and Education Centre, Australia
- Contact Dermatitis, Irritant — Medscape Reference
- Chronic hand eczema — AHA! Swiss Allergy Centre
- Hand dermatitis — British Association of Dermatologists
- Dyshidrotic eczema — American Academy of Dermatology
