Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Dermoscopy of atypical naevi
Created 2008.
Learning objectives
- Describe dermoscopic features of atypical naevi
Introduction
Atypical naevi, Clark's naevi or ‘funny-looking’ moles, are common and are important simulants of melanoma. Melanoma may appear identical clinically and on dermoscopy, requiring biopsy to distinguish them. Stable naevi are much more common than malignant lesions, and so only those at highest risk should be excised. Pathologists may also have difficulty making the diagnosis.
Some authors distinguish ‘dysplastic naevi’ from other atypical naevi (others use the terms synonymously). Dysplastic naevi have at least 3 of the following clinical characteristics:
- Diameter >5 mm
- Ill-defined borders
- Irregular margin
- Varying shades in the lesion
- Papular and macular components
A patient may have a single distinctive dysplastic naevus, or multiple dysplastic naevi. A high grade solitary dysplastic naevus may be difficult to distinguish from melanoma, and is best excised. Multiple dysplastic naevi should be monitored. They may indicate a patient's predisposition to melanoma, particularly if there is a family history of melanoma (atypical mole or dysplastic naevus syndrome). The melanoma may arise from a precursor dysplastic naevus but more often arises de novo.
In this course, the term atypical naevi will encompass a broad range of naevi with unusual clinical and dermoscopic features that are benign on histology.
Dermoscopy of atypical naevi
The dermoscopic features discriminating between atypical naevi and melanoma require expert interpretation and may be misleading. Atypical naevi may have an irregular pattern of pigment distribution but do not reveal specific features of melanoma. However, it can be extremely difficult or impossible to distinguish melanoma from atypical naevus.
The best clues for histological atypia appear to be related to structural features and pigment distribution. Frequently a patient with multiple atypical naevi has a predominance of one type.
Possible structures in atypical naevi include:
- Reticular
- Globular
- Homogeneous
- Reticular/homogeneous
- Globular/homogeneous
- Reticular/globular
The presence of all three types of structure is very suggestive of melanoma. It has also been shown that naevi showing complex dermoscopic pattern are more prevalent in patients who develop melanoma, i.e., naevi in which there are network, globules +/- structureless areas.
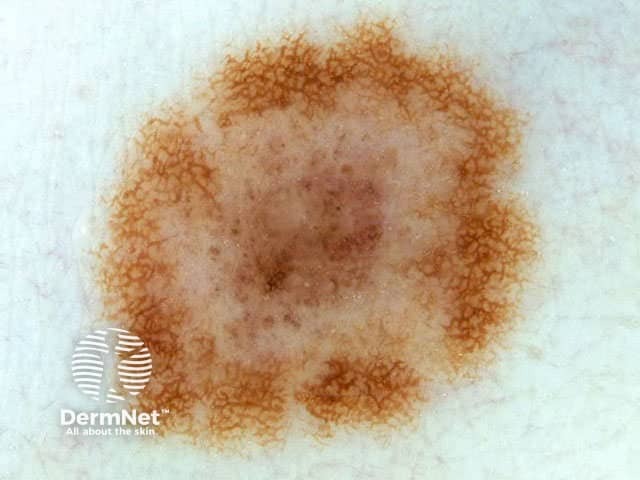
Atypical naevi: structural patterns
Reticular pattern Globular pattern Homogenous pattern Reticular/homogeneous Reticular/homogeneous Globular/homogeneous Globular/homogeneous Reticular/globular 





The distribution of pigmentation may be:
- Uniform
- Central hypopigmented annular type
- Eccentric hypopigmented type
- Central hyperpigmented type (darker skin types)
- Eccentric hyperpigmented type (‘Bolognia naevus’)
- Multifocal hyper-/hypopigmented type
Naevi with central amorphous hyperpigmentation are often seen in midlife and may have a scaly surface. Removing the scale by tape stripping may reveal a reticular pattern.
Atypical naevi: distribution of pigmentation

Uniform pigmentation

Central hypopigmentation

Eccentric hyperpigmentation

Central hyperpigmentation

Eccentric hyperpigmentation
Multifocal pigmentation

Multifocal pigmentation

Asymmetrical pattern
Combined macular and papular components are common features of atypical naevi. The term compound naevus is used if there are junctional and dermal components. The term combined naevus is used when the dermal component is a deeply pigmented blue naevus.
Atypical naevi: combined macular and papular components

Compound naevus

Compound naevus

Naevus with milia-like cysts

Combined naevus
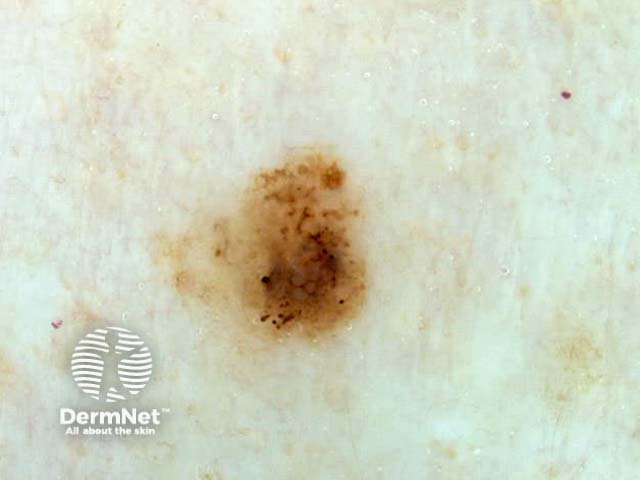
The next few images show naevi that appeared clinically atypical but had benign histology.

Streaming

Asymmetry, 3 colours

Asymmetry, multifocal

Recurrence after shave excision
Other dermoscopic features of atypical naevi may include:
- Dermoscopic regression structures (white scar-like areas and grey peppering)
- Irregular vascular pattern
- Grey-blue areas

Grey peppering

Irregular vascular pattern

Areas of regression

Grey-blue areas
Spitz naevi
Spitz naevi present as evolving lesions and tend to be pink (classic) or black (pigmented or Reed type). They often arise in children and eventually involute. They may be clinically, dermoscopically and histologically difficult to distinguish from melanoma.
Several dermoscopic patterns have been described for Spitz naevi.
- Globular: central grey or bluish pigment surrounded by large peripheral globules
- Starburst: central grey or bluish pigment surrounded by radiating peripheral streaks or globules
- Reticular: superficial dark network
- Homogeneous
- Atypical: irregular blotches, globules and streaks
Spitz naevus

Clinical view

Dermoscopy
Changing naevi
A proportion of benign naevi may be observed to change by dermoscopic monitoring at intervals of months to years. This is particularly likely in childhood, when naevi often change from globular pattern to network pattern and sometimes to a homogeneous structure. Sun exposure may cause globules and dots to disappear or move from the centre to the periphery.
Some changes seen in benign moles are unrelated to malignancy:
- Naevi with peripheral globules may frequently be observed to expand and lose their globules over a period of months.
- Uniform darkening in colour may be observed after sun exposure.
- Naevi may darken during pregnancy.
- The number of milia-like cysts in dermal naevi may vary.
- Naevi fade and disappear slowly in many adults, particularly after the age of 50.
- Trauma may result in inflammation, scabbing and crusting, which resolves within a few weeks.
- Naevi may recur if inadequately excised e.g. by shave biopsy.
Changing common naevi: magnification of images is constant

Images are 15 months apart

Images are a year apart

Images are a year part

Images 2 years apart

Images are 2 years apart

Scab on a mole

Repigmentation in scar
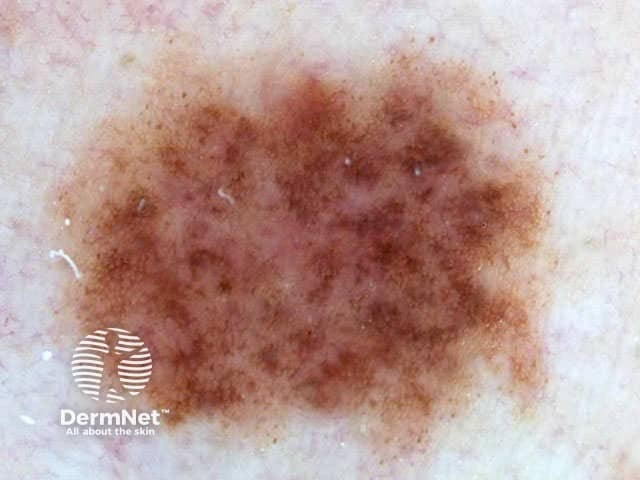
Changing shape, size or structure of flat atypical naevi are more worrying. About 10 to 15% of these will prove to be melanoma. If changes are mild, it may be reasonable to review the dermoscopy in 3 months.
There should be a low threshold for excision in changing atypical naevi that are elevated, because of rapid growth and relatively poor prognosis of nodular melanoma.
Changing atypical naevi

Images are 3 years apart

Images are 3 years apart

Images are 2 years apart

Images are 2 years apart
Activity
Describe the evidence that serial photography with dermoscopy enables early diagnosis of melanoma in patients with atypical naevi.
References
- Hofmann-Wellenhof R, Blum A, Wolf IH, Zalaudek I, Piccolo D, Kerl H, Garbe C, Soyer HP. Dermoscopic classification of Clark's nevi (atypical melanocytic nevi). Clin Dermatol. 2002 May-Jun;20(3):255-8. Medline.
- Wang SQ, Kopf AW, Koenig K, Polsky D, Nudel K, Bart RS. Detection of melanomas in patients followed up with total cutaneous examinations, total cutaneous photography, and dermoscopy. J Am Acad Dermatol. 2005 Jan;50(1):15-20. Medline.
- Menzies SW, Gutenev A, Avramidis M, Batrac A, McCarthy WH. Short-term digital surface microscopic monitoring of atypical or changing melanocytic lesions. Arch Dermatol. 2001 Dec;137(12):1583-9. Medline.
On DermNet
Books about skin diseases
See the DermNet bookstore.
