Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Incontinentia pigmenti — extra information
Incontinentia pigmenti
Author: Vanessa Ngan, Staff Writer, 2005. Updated by Dr Lydia Chan, Dermatology Registrar, Waikato Hospital, Hamilton, New Zealand, 2016.
Introduction Causes Introduction - IKBKG gene Clinical features Cutaneous features Treatment
What is incontinentia pigmenti?
Incontinentia pigmenti is a rare genetic condition characterised by skin, eye, teeth and central nervous system (CNS) abnormalities. The characteristic skin lesions of incontinentia pigmenti are present at birth or develop in the first few weeks of life in approximately 90% of patients.
Incontinentia pigmenti is also referred to as ‘Bloch-Sulzberger syndrome’, ‘Bloch-Siemens syndrome’, ‘melanoblastosis cutis linearis’, and ‘pigmented dermatosis-Siemens-Bloch type’.
What causes incontinentia pigmenti?
Incontinentia pigmenti is a dominant X-linked disease. This means that the abnormal incontinentia pigmenti gene is located on one of the X chromosomes, which determine the sex of a child (XY=male; XX=female). Dominant X-linked disease means that a female with only one copy of the abnormal gene will show the disease, even though they have a normal gene on their other X-chromosome. Males who inherit the abnormal gene do not survive, resulting in miscarriage or stillbirth (X-linked dominant, male-lethal syndrome). Rarely incontinentia pigmenti is reported in males with Klinefelter syndrome (XXY syndrome) or as a result of spontaneous mutations.
The incontinentia pigmenti gene is localised on chromosome Xq28. This gene normally codes for the nuclear factor-KB essential modulator protein and is known as the IKBKG gene (formerly known as NEMO or NF-kappaB gene).
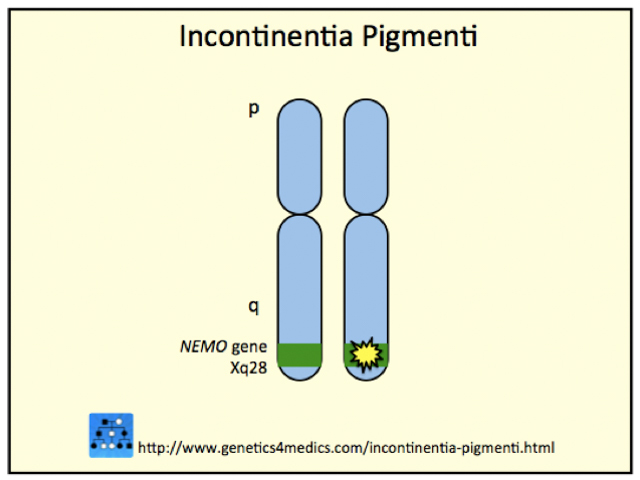
Genetics of Incontinentia pigmenti*
*Image courtesy Genetics 4 Medics
What does the IKBKG gene do?
The IKBKG gene is involved in the regulation of the cell’s division and programmed cell death.
How do mutations in IKBKG cause the symptoms of incontinentia pigmenti?
Mutations in the IKBKG gene prevent it from working, and cells that have the mutation are more prone to programmed cell death.
Cell death in the skin may present with blisters. These heal as the cells with the mutation die and are replaced by surrounding cells.
Cell death also affects the endothelial cells (cells lining blood vessel walls) in the brain. This causes abnormal vessels to develop, and leakage of proteins from the blood into the brain. This may cause seizures.
What are the cutaneous features of incontinentia pigmenti?
Progressive skin rashes are the main clinical feature of the disease. There are four recognised clinical stages but their sequence is irregular, their duration variable and they may overlap.
Stage 1: Vesicular
- Most often affects extremities and scalp but can arise on any part of the body
- Red, blister-like lesions
- Often appear grouped in lines along the arms and legs (following so-called blaschko lines)
- Present at birth or within the first 2 weeks of life in 90% of patients
- May last from a few weeks to a few months and recur throughout the first few months of life

Vesicular stage of incontinentia pigmenti

Vesicular stage of incontinentia pigmenti
Stage 2: Verrucous
- Wart-like or pustular lesions
- Thick crusts or scabs form on top of healing blisters
- Lesions may be darker in skin colour (hyperpigmentation)
- May be present at birth but in 70-80% of patients evolves after the first stage
- May last for months, but rarely longer than a year

Verrucous stage of incontinentia pigmenti
Stage 3: Hyperpigmented
- Skin is darkened in a swirled pattern
- Pigmentation ranges from blue-grey or slate to brown
- Present at birth in 5-10% of patients but usually appears within the first few months of life in 90-98% of patients
- Darkened patches may or may not be related to areas affected in stage 1 and 2
- Heavy pigmentation tends to fade slowly with increasing age

Hyperpigmented stage of incontinentia pigmenti

Hyperpigmented stage of incontinentia pigmenti
Stage 4: Atrophic/ hypopigmented
- Scar-like lesions develop during adolescence and persist into adulthood
- Occur in 30-75% of patients
- Appear as pale, hairless patches or streaks
Other organ involvement
Other organs may be affected in various ways in patients with incontinentia pigmenti. These manifestations may not be seen or recognised until infancy or early childhood.
Teeth
- Abnormalities in more than 80% of patients
- Delay in eruption of teeth (both baby and adult teeth affected)
- Some teeth may be missing altogether
- Teeth may be unusually shaped, typically pegged or cone-shaped
Nails
- May be involved in up to 40% of patients
- Nails may be ridged, pitted, thickened or completely disfigured
- Usually, all or multiple fingernails and toenails are affected
Hair
- Minor hair abnormalities in up to 50% of patients
- Loss or lack of hair on the crown of the head
- Absence of eyebrows and eyelashes
- Hair may be coarse, wiry and lack lustre
Eyes
- Eye defects occur in 20-35% of patients
- Typically occur before age 5
- The disease causes an abnormality in the growth of blood vessels in the inside of the eye resulting in scarring
- Can cause blindness but may be treated if recognised early enough
Central nervous system
- Neurological complications may occur in up to 30% of patients
- The most common complication is seizures which usually develop within the first few weeks of life
- Other manifestations include slow motor development, intellectual disability, spastic paralysis, cerebral atrophy
Other organ systems
- Manifestations are rare
- Skeletal abnormalities such as extra ribs, shortened limb, smaller head circumference and finger abnormalities
- Heart abnormalities
- Lung abnormalities
What is the treatment for incontinentia pigmenti?
There is no specific treatment for incontinentia pigmenti. The main goal is to prevent secondary bacterial infection of skin lesions and to monitor closely the development of related problems. This should include regular dental care and close monitoring by an ophthalmologist for the first few years of life.
References
- OMIM – Online Mendelian Inheritance in Man (search term Incontinentia pigmenti)
- Book: Textbook of Dermatology. Ed Rook A, Wilkinson DS, Ebling FJB, Champion RH, Burton JL. Fourth edition. Blackwell Scientific Publications.
- Conte MI, Pescatore A, Paciolla M, Esposito E, Miano MG, et al. Insight into IKBKG/NEMO locus: report of new mutations and complex genomic rearrangements leading to incontinentia pigmenti disease. Human Mutation [Hum Mutat] 2014 Feb; Vol. 35 (2), pp. 165–77. PubMed
- Hand JL. What's new with common genetic skin disorders? Curr Opin Pediatr. 2015 Aug;27(4):460–5. PubMed
- Jabbari A, Ralston J, Schaffer J. Incontinentia pigmenti. Dermatology Online Journal, 16(11). 2010. PubMed
- Minić S, Trpinac D, Obradović M. Systematic review of central nervous system anomalies in incontinentia pigmenti. Orphanet Journal Of Rare Diseases. 2013(8):25. PubMed
- Paller AS, Mancini AJ. Hurwitz Clinical Pediatric Dermatology 6th Ed.
- Ridder DA, Wenzel J, Müller K, Töllner K, Tong XK et al. Brain endothelial TAK1 and NEMO safeguard the neurovascular unit. J Exp Med. 2015 Sep 21;212(10):1529–49. PubMed
On DermNet
Other websites
- Incontinentia pigmenti — Medscape Reference
- Incontinentia pigmenti US National Library of Medicine Genetics Home Reference
- Incontinentia Pigmenti International Foundation
