Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Paediatric psoriasis — extra information
Paediatric psoriasis
Author: Elizabeth Brown, Medical Student, Waikato Clinical School, Auckland University Faculty of Medical and Health Sciences, 2013.
Introduction
Types
Causes
Diagnosis
Severity assessment
Treatment
Outlook
What is psoriasis?
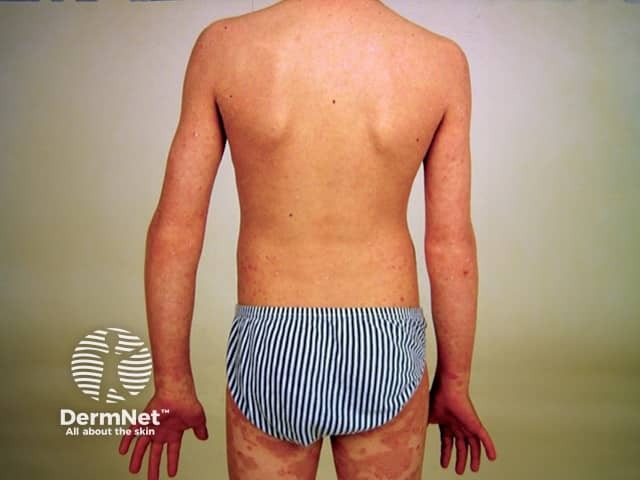
Psoriasis is a chronic skin condition that occurs in children and adults. The typical appearance is of red, thickened, scaly patches on the skin (plaques). These plaques can vary in size and distribution from person to person. In some people, it may affect small areas of skin while others may have large areas covering their body.

Guttate psoriasis in child

Psoriasis in child

Psoriasis in child

Facial psoriasis in child

Scalp psoriasis in child
Erythrodermic psoriasis in child
What kinds of psoriasis occur in children?
Each of the patterns of psoriasis described in adults can be seen in children. These include:
- Flexural psoriasis (red areas between skin folds)
- Scalp psoriasis (thick scales found on areas of the scalp)
- Nail psoriasis (nail dystrophy related to psoriasis)
- Acute guttate psoriasis (small red plaques occurring after an infection)
- Chronic plaque psoriasis (red plaques with scaling occurring anywhere on the body)
- Erythrodermic psoriasis (severe reddening covering most or all of the body)
- Pustular psoriasis (severe pustules that arise acutely)
- Photosensitive psoriasis (affecting areas of sun exposure)
Guttate, facial and flexural psoriasis are particularly common in children.
What causes psoriasis?
Psoriasis has a strong genetic component and is due to abnormal processes involved in the regulation of the immune system.
Individuals may have flares of psoriasis in response to stress, injury, medications and infections (particularly streptococcal tonsillitis).
Psoriasis is not contagious, therefore, affected children do not need to be isolated from other children.
How is the diagnosis made?
The diagnosis of psoriasis is usually made clinically. This involves a doctor examining the skin and making the diagnosis based on the appearance of the affected areas.
- The plaques tend to be distributed symmetrically.
- They favour certain sites such as scalp, elbows and knees; or; skin folds such as behind ears, armpits and groin.
- They are well-circumscribed, red and scaly.
- There is often a family history of psoriasis.
Occasionally, a skin biopsy may be necessary to distinguish psoriasis from other skin conditions that may appear similar.
How is the severity of psoriasis assessed?
Assessing the severity of psoriasis can assist in deciding upon the most appropriate course of treatment. The severity of psoriasis can be determined in the following ways:
- Calculate the body surface area involved
- Estimate a PASI score (psoriasis area and severity index). See also Patient-oriented psoriasis PO-PASI score.
- Use a questionnaire to assess a person’s quality of life eg, the Children’s Dermatology Life Quality Index (CDLQI)
Individuals with severe psoriasis are best managed by a specialist dermatologist. Children and adolescents with psoriasis can experience significant psychological and social effects and may require input from a paediatric dermatologist, paediatrician and counsellors.
What treatment is available for children with psoriasis?
Although there is no cure, several treatment options are available to manage psoriasis.
Topical therapy
Topical therapies are suitable for all children with psoriasis and may be all that is required for mild to moderate psoriasis.
- Vitamin D analogues such as calcipotriol are applied to plaques twice daily
- Topical corticosteroids are available in different potencies and vehicles and are usually used for short courses or no more often than 2-3 times per week long-term
- Dithranol preparations are usually used short-contact
- but are tricky to use because they stain and can irritate the skin
- Coal tar may be suitable for use in children with psoriasis that does not affect the face or genitals. It is especially useful for scalp psoriasis, but many children dislike the odour.
Phototherapy
Narrowband UVB phototherapy is often used in children with psoriasis, especially in those over 10 years of age. Thin chronic plaque psoriasis and guttate psoriasis respond best. A hospital-based course of treatment usually requires attendance 3 times weekly for 6 to 12 weeks. Broadband UVB and PUVA are available in some centres.
Methotrexate
Methotrexate tablets prescribed off-label once weekly are useful in children that have not improved satisfactorily with topical preparations or phototherapy. The data on the use of methotrexate is less extensive in children compared to adults. However, several case reports have shown significant clinical improvement in children as young as 2 years old, with excellent tolerance. Regular blood tests are required to monitor safety.
Biologic agents
Biologic agents (e.g. subcutaneous etanercept and intravenous infliximab injections) should only be used in children with severe psoriasis that does not respond to other therapies. Biologics are considered to be safe in children although serious adverse effects (especially infection) have been reported. Use of a biological agent will be made in consultation with a dermatologist on a case by case basis.
What is the outlook for children with psoriasis?
Psoriasis in children may completely clear up within months of presentation, especially if guttate plaques occur in response to an infection. However, some children progress to have long-term psoriasis, often life-long. Early-onset large chronic plaque psoriasis tends to be particularly persistent and challenging to treat. Complications such as psoriatic arthritis and non-alcoholic fatty liver disease may occur.
Children with severe psoriasis should be advised to maintain a healthy weight, take regular exercise, and to avoid smoking.
Bibliography
- Marji JS, Marcus R, Moennich J, Mackay-Wiggan J. Use of biologic agents in pediatric psoriasis. J Drugs Dermatol. 2010;9(8):975–86. PubMed
- Napolitano M, Megna M, Balato A, et al. Systemic treatment of pediatric psoriasis: a review. Dermatol Ther (Heidelb). 2016;6(2):125–42. doi:10.1007/s13555-016-0117-6. PubMed
- Relvas M, Torres T. Pediatric psoriasis. Am J Clin Dermatol. 2017;18(6):797–811. doi:10.1007/s40257-017-0294-9. PubMed
- Mahé E. Childhood psoriasis. Eur J Dermatol. 2016;26(6):537–48. doi:10.1684/ejd.2016.2932. PubMed
- Eichenfield LF, Paller AS, Tom WL, et al. Pediatric psoriasis: evolving perspectives. Pediatr Dermatol. 2018;35(2):170–81. doi:10.1111/pde.13382. PubMed
- Bronckers IM, Paller AS, van Geel MJ, van de Kerkhof PC, Seyger MM. Psoriasis in children and adolescents: diagnosis, management and comorbidities. Paediatr Drugs. 2015;17(5):373–84. doi:10.1007/s40272-015-0137-1. PubMed
- Bronckers IMGJ, Paller AS, West DP, et al. A comparison of psoriasis severity in pediatric patients treated with methotrexate vs biologic agents. JAMA Dermatol. 2020;156(4):384–92. doi:10.1001/jamadermatol.2019.4835. PubMed
- Sanclemente G, Murphy R, Contreras J, García H, Bonfill Cosp X. Anti-TNF agents for paediatric psoriasis. Cochrane Database Syst Rev. 2015;2015(11):CD010017. doi:10.1002/14651858.CD010017.pub2. PubMed
On DermNet
Other websites
- I'm Just Like You – Children with Psoriasis – YouTube video from National Psoriasis Foundation
- MyPsoriasis.co.nz – Information for New Zealand patients with psoriasis and psoriatic arthritis, sponsored by AbbVie
