Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Basal cell carcinoma — extra information
Basal cell carcinoma
Author: Honorary Associate Professor Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1997. Updated December 2015.
Introduction
Demographics
Causes
Clinical features
Types of BCC
Complications
Diagnosis
Treatment for primary basal cell carcinoma
Treatment for advanced basal cell carcinoma
Prevention
Outlook
What is basal cell carcinoma?
Basal cell carcinoma (BCC) is a common, locally invasive, keratinocyte cancer (also known as nonmelanoma cancer). It is the most common form of skin cancer. BCC is also known as rodent ulcer and basalioma. Patients with BCC often develop multiple primary tumours over time.
Who gets basal cell carcinoma?
Risk factors for BCC include:
- Age and sex: BCCs are particularly prevalent in elderly males. However, they also affect females and younger adults
- Previous BCC or other form of skin cancer (squamous cell carcinoma, melanoma)
- Sun damage (photoageing, actinic keratoses)
- Repeated prior episodes of sunburn
- Fair skin, blue eyes and blond or red hair — note; BCC can also affect darker skin types
- Previous cutaneous injury, thermal burn, disease (eg cutaneous lupus, sebaceous naevus)
- Inherited syndromes: BCC is a particular problem for families with basal cell naevus syndrome (Gorlin syndrome), Bazex-Dupré-Christol syndrome, Rombo syndrome, Oley syndrome and xeroderma pigmentosum
- Other risk factors include ionising radiation, exposure to arsenic, immune suppression due to disease or medicines, and use of some other medicines such as hydrochlorothiazide.
What causes basal cell carcinoma?
The cause of BCC is multifactorial.
- Most often, there are DNA mutations in the patched (PTCH) tumour suppressor gene, part of hedgehog signalling pathway.
- These may be triggered by exposure to ultraviolet radiation.
- Various spontaneous and inherited gene defects predispose to BCC.
What are the clinical features of basal cell carcinoma?
BCC is a locally invasive skin tumour. The main characteristics are:
- Slowly growing plaque or nodule
- Skin coloured, pink or pigmented
- Varies in size from a few millimetres to several centimetres in diameter
- Spontaneous bleeding or ulceration.
BCC is very rarely a threat to life. A tiny proportion of BCCs grow rapidly, invade deeply, and/or metastasise to local lymph nodes.
Types of basal cell carcinoma
There are several distinct clinical types of BCC, and over 20 histological growth patterns of BCC.
Nodular BCC
- Most common type of facial BCC
- Shiny or pearly nodule with a smooth surface
- May have central depression or ulceration, so its edges appear rolled
- Blood vessels cross its surface
- Cystic variant is soft, with jelly-like contents
- Micronodular, microcystic and infiltrative types are potentially aggressive subtypes
- Also known as nodulocystic carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma
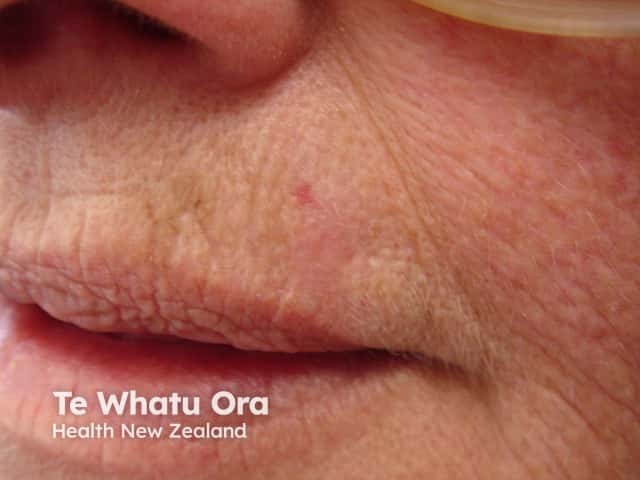
Superficial BCC
- Most common type in younger adults
- Most common type on upper trunk and shoulders
- Slightly scaly, irregular plaque
- Thin, translucent rolled border
- Multiple microerosions

Basal cell carcinoma

Superficial basal cell carcinoma

Superficial basal cell carcinoma, face

Superficial basal cell carcinoma, back
Morphoeic BCC
- Usually found in mid-facial sites
- Waxy, scar-like plaque with indistinct borders
- Wide and deep subclinical extension
- May infiltrate cutaneous nerves (perineural spread)
- Also known as morpheic, morphoeiform or sclerosing BCC

Morphoeic basal cell carcinoma

Morphoeic basal cell carcinoma

Morphoeic basal cell carcinoma
Morphoeic basal cell carcinoma
Basosquamous carcinoma
- Mixed basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)
- Infiltrative growth pattern
- Potentially more aggressive than other forms of BCC
- Also known as basosquamous carcinoma and mixed basal-squamous cell carcinoma

Basal cell carcinoma

Basisquamous cell carcinoma

Basisquamous cell carcinoma
See more images of basal cell carcinoma.
- BCC affecting the face images
- BCC affecting the nose images
- BCC affecting the eyelid images
- BCC affecting the ear images
- BCC affecting the trunk images
Complications of basal cell carcinoma
Recurrent BCC
Recurrence of BCC after initial treatment is not uncommon. Characteristics of recurrent BCC often include:
- Incomplete excision or narrow margins at primary excision
- Morphoeic, micronodular, and infiltrative subtypes
- Location on head and neck.

After PDT

After superficial surgery

After fluorouracil

After imiquimod
Advanced BCC
Advanced BCCs are large, often neglected tumours.
- They may be several centimetres in diameter
- They may be deeply infiltrating into tissues below the skin
- They are difficult or impossible to treat surgically
Metastatic BCC
- Very rare
- Primary tumour is often large, neglected or recurrent, located on head and neck, with aggressive subtype
- May have had multiple prior treatments
- May arise in site exposed to ionising radiation
- Can be fatal
How is basal cell carcinoma diagnosed?
BCC is diagnosed clinically by the presence of a slowly enlarging skin lesion with typical appearance. The diagnosis and histological subtype is usually confirmed pathologically by a diagnostic biopsy or following excision.
Some typical superficial BCCs on trunk and limbs are clinically diagnosed and have non-surgical treatment without histology.
What is the treatment for primary basal cell carcinoma?
The treatment for a BCC depends on its type, size and location, the number to be treated, patient factors, and the preference or expertise of the doctor. Most BCCs are treated surgically. Long-term follow-up is recommended to check for new lesions and recurrence; the latter may be unnecessary if histology has reported wide clear margins.
Excision biopsy
Excision means the lesion is cut out and the skin stitched up.
- Most appropriate treatment for nodular, infiltrative and morphoeic BCCs.
- Should include 3 to 5 mm margin of normal skin around the tumour.
- Very large lesions may require flap or skin graft to repair the defect.
- Pathologist will report deep and lateral margins.
- Further surgery is recommended for lesions that are incompletely excised.
Mohs micrographically controlled excision
Mohs micrographically controlled surgery involves examining carefully marked excised tissue under the microscope, layer by layer, to ensure complete excision.
- Very high cure rates achieved by trained Mohs surgeons.
- Used in high-risk areas of the face around eyes, lips and nose.
- Suitable for ill-defined, morphoeic, infiltrative and recurrent subtypes.
- Large defects are repaired by flap or skin graft.
Superficial skin surgery
Superficial skin surgery comprises shave, curettage, and electrocautery. It is a rapid technique using local anaesthesia and does not require sutures.
- Suitable for small, well-defined nodular or superficial BCCs.
- Lesions are usually located on trunk or limbs.
- Wound is left open to heal by secondary intention.
- Moist wound dressings lead to healing within a few weeks.
- Eventual scar quality variable.
Cryotherapy
Cryotherapy is the treatment of a superficial skin lesion by freezing it, usually with liquid nitrogen.
- Suitable for small superficial BCCs on covered areas of trunk and limbs.
- Best avoided for BCCs on head and neck, and distal to knees.
- Double freeze-thaw technique.
- Results in a blister that crusts over and heals within several weeks.
- Leaves permanent white mark.
Photodynamic therapy
Photodynamic therapy (PDT) refers to a technique in which BCC is treated with a photosensitising chemical, and exposed to light several hours later.
- Topical photosensitisers include aminolevulinic acid lotion and methyl aminolevulinate cream.
- Suitable for low-risk small, superficial BCCs.
- Best avoided if tumour in site at high risk of recurrence.
- Results in inflammatory reaction, maximal 3–4 days after procedure.
- Treatment repeated 7 days after initial treatment.
- Excellent cosmetic results.
Imiquimod cream
Imiquimod is an immune response modifier.
- Best used for superficial BCCs less than 2 cm diameter.
- Applied three to five times each week, for 6–16 weeks.
- Results in a variable inflammatory reaction, maximal at three weeks.
- Minimal scarring is usual.
Fluorouracil cream
5-Fluorouracil cream is a topical cytotoxic agent.
- Used to treat small superficial basal cell carcinomas.
- Requires prolonged course, eg twice daily for 6–12 weeks.
- Causes inflammatory reaction.
- Has high recurrence rates.
Radiotherapy
Radiotherapy or X-ray treatment can be used to treat primary BCCs or as adjunctive treatment if margins are incomplete.
- Mainly used if surgery is not suitable.
- Best avoided in young patients and in genetic conditions predisposing to skin cancer.
- Best cosmetic results achieved using multiple fractions.
- Typically, patient attends once-weekly for several weeks.
- Causes inflammatory reaction followed by scar.
- Risk of radiodermatitis, late recurrence, and new tumours.
What is the treatment for advanced or metastatic basal cell carcinoma?
Locally advanced primary, recurrent or metastatic BCC requires multidisciplinary consultation. Often a combination of treatments is used.
- Surgery
- Radiotherapy
- Targeted therapy.
Targeted therapy refers to the hedgehog signalling pathway inhibitors, vismodegib and sonidegib. These drugs have some important risks and side effects.
How can basal cell carcinoma be prevented?
The most important way to prevent BCC is to avoid sunburn. This is especially important in childhood and early life. Fair skinned individuals and those with a personal or family history of BCC should protect their skin from sun exposure daily, year-round and lifelong.
- Stay indoors or under the shade in the middle of the day.
- Wear covering clothing.
- Apply high protection factor SPF50+ broad-spectrum sunscreens generously to exposed skin if outdoors.
- Avoid indoor tanning (sun beds, solaria).
Oral nicotinamide (vitamin B3) in a dose of 500 mg twice daily may reduce the number and severity of BCCs.
What is the outlook for basal cell carcinoma?
Most BCCs are cured by treatment. Cure is most likely if treatment is undertaken when the lesion is small.
About 50% of people with BCC develop a second one within 3 years of the first. They are also at increased risk of other skin cancers, especially melanoma. Regular self-skin examinations and long-term annual skin checks by an experienced health professional are recommended.
References
- Guidelines for the Management of Basal Cell Carcinoma (NR Telfer, GB Colver, PW Bowers). BJD, Vol. 159, No.1, July 2008 (p35) — British Association of Dermatologists
- Kim JY, Kozlow JH, Mittal B, Moyer J, Olencki T, Rodgers P. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018 Mar;78(3):540–59. doi: 10.1016/j.jaad.2017.10.006. PubMed
On DermNet
- Basal cell carcinoma pathology
- Dermatological procedures
- Mohs micrographic surgery
- Skin lesions
- Skin cancer
- Gorlin syndrome
- Bazex syndrome
- Genetics of basal cell carcinoma
- Basal cell carcinoma — common skin lesions course
- Vulval cancer
- Melanoma in skin of colour
- Ultraviolet radiation
- Targeted therapy
Other websites
- Skin cancers and precancers — DermNet e-lecture [Youtube]
- Cancer Council Australia
- Clinical practice guidelines for keratinocyte cancer — Cancer Guidelines wiki
- American College of Mohs Micrographic Surgery and Oncology
- Mohs Micrographic Surgery from Johns Hopkins Oncology Center
- Basal cell carcinoma: emedicine dermatology, the online medical reference textbook.
- Basal cell carcinoma — British Association of Dermatologists
- Optimal care pathway for people with basal cell carcinoma or squamous cell carcinoma — Cancer Council of Australia, June 2016
- Basal cell carcinoma — American Academy of Dermatology
