Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Postinflammatory hyperpigmentation — extra information
Postinflammatory hyperpigmentation
Author: Vanessa Ngan, Staff Writer, 2005. Updated by A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, December 2015.
Introduction Demographics Causes Clinical features Diagnosis Treatment
What is postinflammatory hyperpigmentation?
Postinflammatory pigmentation is temporary pigmentation that follows injury (eg, a thermal burn) or inflammatory disorder of the skin (eg, dermatitis, infection). It is mostly observed in darker skin types (see ethnic dermatology). Postinflammatory pigmentation is also called acquired melanosis.
More severe injury results in postinflammatory hypopigmentation, which is usually permanent.
Who gets postinflammatory pigmentation?
Postinflammatory hyperpigmentation can occur in anyone but is more common in darker-skinned individuals, in whom the colour tends to be more intense and persist for a longer period than in lighter skin colours. Pigmentation tends to more pronounced in sun-induced skin conditions such as phytophotodermatitis and lichenoid dermatoses (skin conditions with lichen planus-like inflammation, such as erythema dyschromicum perstans).
Some medications may also darken postinflammatory pigmentation. These include antimalarial drugs, clofazimine, tetracycline, anticancer drugs such as bleomycin (flagellate erythema), doxorubicin, 5-fluorouracil and busulfan.
What causes postinflammatory hyperpigmentation?
Postinflammatory hyperpigmentation follows damage to the epidermis and/or dermis with deposition of melanin within the keratinocytes (skin cells) and/or dermis.
Inflammation in the epidermis stimulates melanocytes to increase melanin synthesis and to transfer the pigment to surrounding keratinocytes (epidermal melanosis). If the basal layer is injured (e.g. lichen planus), melanin pigment is released and subsequently trapped by macrophages in the papillary dermis (dermal melanosis or pigment incontinence).
What are the clinical features of postinflammatory hyperpigmentation?
Postinflammatory hyperpigmented patches are located at the site of the original disease after it has healed. The lesions range from light brown to black in colour. The patches may become darker if exposed to sunlight (UV rays).

Lichen planus actinicus

Violin playing (friction)

Irritant dermatitis

Postinflammatory hyperpigmentation (inflamed cyst)

Oven burn

Photodynamic therapy

Flagellate reaction to bleomycin
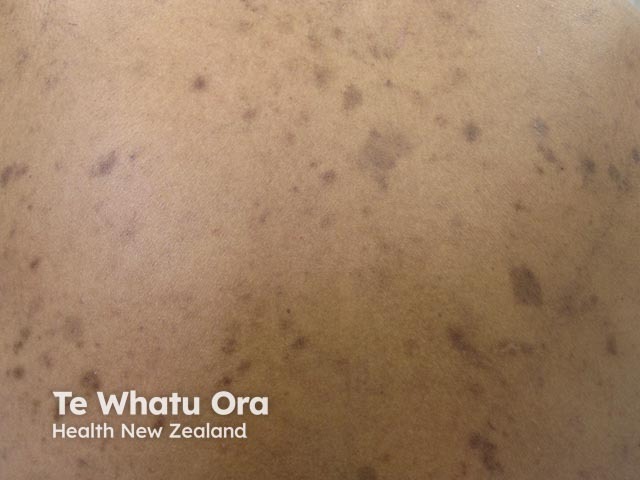
Healed eczema
How is postinflammatory hyperpigmentation diagnosed?
Postinflammatory hyperpigmentation is diagnosed by taking a careful history and examining the skin. Dermal melanosis gives a characteristic hue to the skin colour (grey-purple-brown).
Sometimes the diagnosis is only made after skin biopsy. Histopathology reveals patchy epidermal melanosis and/or dermal melanosis.
What is the treatment for postinflammatory hyperpigmentation?
If pigmentation affects an exposed site, daily application of SPF 50+ broad-spectrum sunscreen is important to minimise darkening caused by UVR. Cosmetic camouflage can be used.
Topical treatments for postinflammatory hyperpigmentation
A variety of topical treatments are available to lighten/bleach hyperpigmented lesions in epidermal hypermelanosis. Varying degrees of success are achieved but combinations of the treatments below are usually required for significant improvement.
- Hydroquinone
- Azelaic acid
- Cysteamine cream
- Vitamin C cream
- Tretinoin cream
- Corticosteroid creams
- Glycolic acid peels
- Others: kojic acid, arbutin, licorice extracts, mequinol, niacinamide, N-acetyl glucosamine, soy
Physical treatments for postinflammatory hyperpigmentation
Chemical peels, laser treatments and intense pulsed light therapies (IPL) may be helpful for epidermal pigmentation, but physical treatments may also aggravate it by injuring the epidermis.
These treatments are not effective in dermal hypermelanosis.
References
- Cardinali G, Kovacs D, Picardo M. Mechanisms underlying post-inflammatory hyperpigmentation: lessons from solar lentigo. Ann Dermatol Venereol. 2012 Dec;139 Suppl 4:S148–52. doi: 10.1016/S0151-9638(12)70127-8. Review. PubMed PMID: 23522630.
- Lamel SA, Rahvar M, Maibach HI. Postinflammatory hyperpigmentation secondary to external insult: an overview of the quantitative analysis of pigmentation. Cutan Ocul Toxicol. 2013 Mar;32(1):67–71. doi: 10.3109/15569527.2012.684419. Epub 2012 Jun 6. Review. PubMed PMID: 22667459.
- Book: Textbook of Dermatology. Ed Rook A, Wilkinson DS, Ebling FJB, Champion RH, Burton JL. Fourth edition. Blackwell Scientific Publications.
- Callender VD, St Surin-Lord S, Davis EC, Maclin M. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011 Apr 1;12(2):87–99. doi: 10.2165/11536930-000000000-00000. Review. PubMed PMID: 21348540
On DermNet
- Skin pigmentation
- Acquired dermal macular hyperpigmentation
- Bleaching creams
- Procedures to treat the skin
- Flagellate erythema
- Melanoma in skin of colour
- Skin signs of rheumatic disease
- Antimalarial medications in dermatology
Other websites
- Postinflammatory Hyperpigmentation — Medscape Reference
